This is an automatically translated article.
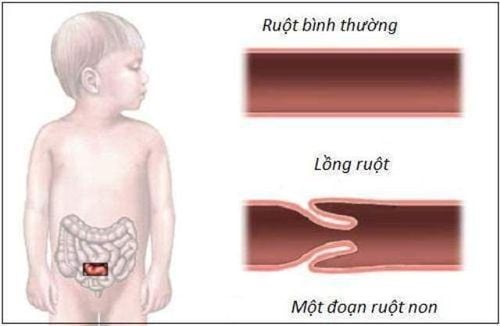
Acute intussusception is a pathological state in which the two upper and lower intestines intertwine, causing mechanical intestinal obstruction syndrome, creating an intussusception of the intestinal lumen, rapid bowel necrosis. The following article focuses on the characteristics, recognition and treatment of acute intussusception in breastfed infants.Intussusception is the most common cause of small bowel obstruction in children under two years of age. It occurs when a segment of the small intestine is invaded or obstructed in the distal bowel, leading to edema of the bowel wall and venous obstruction. Approximately 74 intussusceptions per 100,000 neonates occur annually worldwide. The incidence has been reported to be high in Vietnam and Korea with 300 per 100,000 live births and low in Bangladesh with 9 per 100,000 births.
Usually, acute intussusception presents with vomiting, abdominal cramps, and bloody stools if hospital admission is delayed. To approach the final diagnosis, several imaging tests may be performed such as ultrasound, abdominal X-ray, barium study, and computed tomography in rare cases.
Some children with intussusception may resolve on their own. However, persistent small bowel intussusception can cause intestinal obstruction or necrosis and requires surgical intervention. If acute intussusception is not detected and treated promptly, the artery that supplies blood to the intestines can become blocked, causing infarction and perforation. Untreated intussusception is a condition that can worsen or even cause death. Therefore, the physician should recognize such cases as soon as possible and prescribe the correct treatment.
Recently, patients are often hospitalized in the early stages with mild symptoms, including abdominal pain and vomiting. Therefore, the definitive diagnosis is mainly based on ultrasound findings, and the pediatric surgeon should decide whether to bring the infant for decompression or close monitoring. In addition, the choice of intervention between saline enema and pneumatic reduction for the treatment of acute intussusception is still debated due to the different success rates from 83%-88%. It is estimated that 80% of intussusception occurs in children under 2 years of age, most often at the age of 5 - 10 months, rarely in older children. Intussusception is more common in boys than girls with a ratio of 2:1.
1. Causes of intussusception in breastfed infants
Acute intussusception is a very common surgical disease and a cause of intestinal obstruction in young children, especially breastfed infants. This is a pathological phenomenon when the upper intestine moves abnormally, burrows into the lower intestine, obstructing intestinal circulation. Here are some causes of intussusception in breastfed infants:1.1. By cause Primary intussusception usually occurs in breastfed infants. Associated with upper respiratory tract disease caused by a virus called Adenovirus. This virus causes inflammation of the mesenteric lymph nodes, mainly in the ileum, and lymphadenitis will increase intestinal motility - one of the favorable factors facilitating intussusception often occurs in the ileum - cecum. This explains why intussusception often occurs at the peak of the virus epidemic season. Secondary intussusception: Occurs in about 10% of all cases. With this type, the researchers found several physical lesions that cause intussusception such as benign or malignant tumors of the intestine, intestinal malformations (double bowel, Meckel's diverticulum...). Postoperative intussusception: This is a complication after abdominal surgery in children especially after surgery of the diaphragm or surgery for diaphragmatic hernia. 1.2. According to the degree of progression Acute intussusception: Occurs mainly in breastfed infants. The disease often progresses rapidly and leads to many dangerous complications such as intestinal obstruction, intestinal necrosis, peritonitis, and toxicity. This is also one of the most common abdominal emergencies, especially in nursing infants. Subacute intussusception: Occurs in older children (3-15 years). The progression is slower, rarely causing complications of intestinal obstruction and bowel necrosis. Chronic intussusception: Occurs in adults or the elderly. Slow progression, potentially self-limiting but often recurrent, often due to colon tumors. low risk of bowel necrosis. In the scope of this article we focus mainly on the types of acute intussusception in breastfed infants.
Lồng ruột cấp ở trẻ bú mẹ rất thường gặp và là nguyên nhân gây tắc ruột
2. Symptoms of intussusception in nursing infants
Intussusception is a medical emergency. If you think your child may have this disorder, see your child's health care provider right away.The symptoms of each child are not the same. The most common symptom is a sudden loud crying while playing or feeding. This is due to sudden, severe abdominal pain in an otherwise healthy child.
This abdominal pain occurs frequently. At first it seemed to be a stomach ache. An infant or child may be tense, knee up, be very irritable, and cry loudly. Your child may feel more comfortable and play in between attacks. Or your baby may become tired and weak from fussiness.
Other symptoms include:
Vomiting Bloody stools Red, jelly-like stools Fever Extreme fatigue or coma Diarrhea Sweating Dehydration Distended abdomen Symptoms of intussusception can be assessed confused with other health problems. It is better to take your child to the medical center for an accurate diagnosis.
3. Diagnosis of intussusception in children
The doctors will review your child's medical history and run several laboratory tests to check the organs in the abdomen. These tests may include:Abdominal X-ray: A diagnostic test that may show an intestinal obstruction. Ultrasound: uses high-frequency sound waves and a computer to create images of blood vessels, tissues, and organs. Ultrasound is used to see organs as they work and to check blood flow through different vessels. Upper GI chain or barium swallow: This test looks at the organs of the top part of the digestive system. It examines the food pipe (esophagus), stomach, and the first part of the small intestine (duodenum). Your child will swallow a metallic liquid called barium. Barium is a form of contrast material that allows the doctor to see the intestines on an X-ray film. Then, X-rays are taken to examine the digestive organs. Barium enema or lower GI series: This is an X-ray examination of the rectum, large intestine, and lower part of the small intestine. Your child will be given a contrast dye called barium. Barium is inserted into a tube and inserted into your child's rectum as an enema. An X-ray of the abdomen will show if there are any narrowed areas called stenosis, any blockages, or other problems. In some cases, intussusception corrects itself during this examination. The intestines may return to their original position on their own. This can happen because of pressure on the intestines while the barium is inserted.

Lồng ruột cấp tính có biểu hiện nôn, đau bụng quặn
4. Management of acute intussusception in breastfed infants
Which way to treat depends on your child's symptoms, age, general health, and the severity of the intussusception.4.1 Removal of the intussusception by air injection (applied a lot in Vietnam) Indications: For all cases of acute intussusception within 24 hours from the onset of symptoms. Very limited to those who come in between 24 - 48 hours with no symptoms. Action: Use a closed inflator with pressure monitoring (mmHg). Manual adjustment method or automatic adjustment method (with telescopic machine) can be used. The maximum pump pressure is 100mmHg. The pressure is too high compared to this pressure, bowel rupture is very likely to occur. The child must be given good pre-anesthesia or intravenous sedation during the procedure to avoid sudden pressure spikes due to the child struggling and pushing. After 3 cycles of pumping to maximum pressure, if unsuccessful, the procedure should be discontinued and surgery should be considered. Evaluation Evaluate the results, if the removal is successful:
The pressure of the meter drops suddenly. The patient's abdomen is flat and round. Pump pressure is not rising or rising very slowly. Deflate the patient's abdomen without collapsing. Palpation of the abdomen no longer shows the tuft of the cage. To test right on the table, you can put a gastric tube and the tip of the tube dipped in a glass of water. When the intestine is removed, it will go back up to the stomach and bubble out in the glass.
After removing the incubator: + X-rays are taken slightly through the small intestine in the shape of a honeycomb.
+ Abdominal ultrasound no longer shows bunions.
+ Give activated charcoal or black stools to the child after 12 hours.
+ The child is pain free, plays again, sucks without vomiting, defecates normally.
Complications due to air intubation. Intestinal rupture: Due to excess pressure above the safe level, children appear cyanosis, respiratory failure, respiratory arrest due to compression of the diaphragm.
4.2 Detachment by hydrostatic pressure (or used in developed countries) Sometimes the intussusception will resolve on its own when the child is given a barium enema. In many cases, doctors can correct the problem by administering an enema with gas or saline solution. This is done by placing a small tube into your child's rectum. Your doctor will use ultrasound or X-rays (fluoroscopy) to help place the tube. Air is introduced into the tube. Airflow can help return the bowels to a normal position. But if your child is very ill from an abdominal infection or other problems, the doctors will consider whether or not to do so.
Disadvantage: long time to remove the intubation will cost the patient, eat a lot of rays and the success rate is low due to uncontrolled pressure. 4.3 Surgical intubation Your child will need surgery if the intussusception is not corrected with a barium enema. Or your child will also need surgery if barium, saline or air enema is not possible. For the surgery, your child will be under anesthesia. The surgeon will perform laparoscopic or brake surgery depending on the case to find the intussusception and push parts of the intestine back into place. The intestines will be examined for damage. If any part is not working properly, they will be cut off.
If your child's intestines are damaged and the section cut out is small, the two healthy sections of intestine will be stitched back together.
In rare cases, a large amount of bowel may be removed. This happens if the intestine is badly damaged. In this case, surgery cannot link the remaining parts of the intestine together after the damaged part is removed. An ileostomy may be performed so that digestion can continue. With an ileostomy, the remaining two healthy ends of the intestine are inserted through openings in the abdomen. The stool will pass through the opening (stomata). It then collects in a bag outside the body. An ileostomy may be short-term. Or in very rare cases, it can be permanent or permanent. It depends on how much bowel has been removed.

Nhiễm trùng đường ruột là một trong các biến chứng của lồng ruột cấp ở trẻ bú mẹ
5. Complications of acute intussusception in breastfed infants
Intussusception is a medical emergency. It is a life-threatening disease. If left untreated, it can cause serious problems such as:Intestinal infections Death after bowel surgery Severe intra-abdominal bleeding or peritonitis.
6. Monitoring at home
After your child is treated for intussusception, it is important that you carefully monitor his or her health. Call the doctor if your child has any of the following symptoms:Fever over 38.3 degrees Any signs of infection, including: redness, swelling, heat, yellow/green discharge from the incision or wound. This is especially important for children who have had surgery. Vomiting Diarrhea or jelly-like stools Intermittent, cramping and abdominal pain If any of these signs are present, take your child to the nearest medical facility immediately for prompt diagnosis and treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.













