This is an automatically translated article.
You have heard of vertebroplasty by biological cement injection (polymethylmethacrylate, PMMA) in the treatment of spinal diseases or solving the problem of spine disease in bone metastatic cancer. Wondering how the process is done? The following article will give you general information about what is vertebroplasty and how is it done?
1. What is vertebroplasty?
Spondyloplasty and spondyloplasty are minimally invasive surgical procedures performed under general anesthesia in an outpatient setting. These procedures are almost always performed in people with metastatic bone cancer and spinal disease; Rarely, they can be done in children.
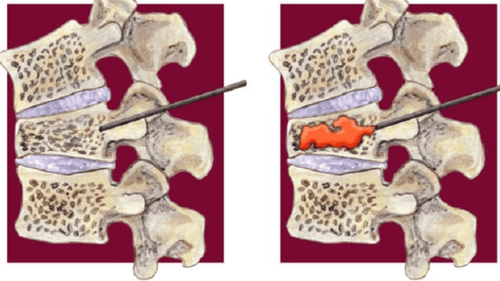
Both vertebroplasty and spondyloplasty involve injecting a cement called polymethylmethacrylate (PMMA) into the broken bone. Kyphoplasty involves the additional step of inserting and inflating a balloon before injecting the cement. Most patients go home immediately after either procedure.
Both surgeries were performed with the help of fluoroscopy, a type of medical imaging technique in which a beam of X-rays is passed through the body. This imaging technique helps guide the surgeon as they operate.
1.1. Percutaneous vertebroplasty treatment for vertebral collapse Percutaneous vertebroplasty, also known as spinal cementation, is a technique of injecting into the collapsed vertebral body the bio-cement solution (Methylmethacrylate) through a tube. A catheter (Troca) is punctured through the skin under the skin viewed on television radiographs without the need for surgery. This technique was first conducted in France and by Professor H. Deramond in 1984. Currently, this technique is being widely applied in many advanced countries in the world.
For the purpose:
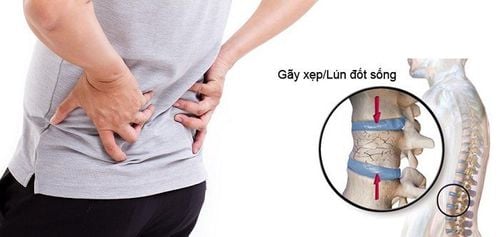
Pain relief effect. The effect of stabilizing the vertebral body. Preoperative hemostasis. 1.2. Fracture of vertebral collapse due to osteoporosis causing pain or collapse due to trauma Tumor lesions causing destruction of the vertebral body (vertebral metastasis with osteolytic, multiple myeloma, eosinophilic granulomatosis).
2. The process of performing vertebroplasty.
Made by 2 main techniques:
2.1. Vertebroplasty: The surgeon will use a specialized needle to poke the vertebral body and inject cement. Bio-cement helps stabilize the vertebral body, and thereby reduces pain for patients. But after pumping, the collapsed vertebrae have not returned to their original shape because the pumping pressure is not enough to expand the vertebrae. And sometimes because the vertebra has collapsed too badly, under the pressure of the pump, the cement can spill out of the vertebrae.
2.2. Kyphoplasty is the most modern technique today, has been widely applied in many advanced countries in the world. After the patient is anesthetized, the surgeon will insert a special needle with a balloon tip into the vertebral body under the guidance of a fluorescent screen. And the balloon will be inflated to expand the vertebrae and return to its original shape. Cement will be injected into the space just created in the spine after the ball is withdrawn, without pressure. So cement is very unlikely to spill out. The vertebrae, after returning to their original shape, will avoid the risk of hunchback and spondylolisthesis for the patient in the future.
This technique has overcome all the disadvantages of Vertebroplasty, while still stabilizing the vertebral body, reducing pain for the patient.
2.3. The vertebroplasty surgery is carried out with quite simple procedures: The patient is placed prone on the operating table. Local anesthetic is injected into the skin where the vertebrae are injured. At that location, a needle about 2mm in diameter is inserted into the broken vertebra. Liquid cement is injected into the vertebrae, overflowing into the fracture lines and when it dries, the cement will bind the broken bone fragments together to form a block, no longer being displaced when moving. After 5-7 minutes, when the cement dries, the needle is withdrawn. After about 6 hours, the patient can sit, get up or walk if there is no paralysis from before surgery.
2.4. Fractured vertebrae with bio-cement has a number of advantages: The technique is simple and gentle, requiring only anesthesia without anesthesia. Rapid pain relief, short hospital stay and recovery time (average 1 night, discharged the next day). For cases of vertebral fractures due to osteoporosis, this is the most effective solution in fast pain relief for patients.
3. Features to pay attention to when shaping vertebrae.
3.1. Contraindications to bio-cement vertebroplasty Absolute contraindications to vertebral plasty or spondyloplasty include patients with the following conditions:
Fracture or vertebral fracture without symptoms improved with conservative measures (eg, rest and pain medication) Uncontrolled bleeding disorder Allergic to bone cement A tumor involving the spinal canal In situ (vertebral body) ) or systemic infection Additional contraindications include patients with back pain unrelated to a vertebral fracture, such as a herniated disc or spinal stenosis. Imaging tests, like magnetic resonance imaging (MRI) of the spine, can help your doctor confirm the correct diagnosis.
3.2. Potential Risks Spondyloplasty and spondyloplasty are generally considered safe, low-risk procedures. However, in rare cases, serious complications can occur.
These complications include:
Infection Bleeding Cementum (PMMA), which can lead to pain, tingling, numbness, or weakness (this is more common for vertebroplasty than blepharoplasty. by kyphoplasty) Pulmonary embolism due to cement particles traveling to the lungs (rare) Spinal stenosis due to cement leak into the epidural space (rare) Damage to nerve roots or spinal cord leading to paralysis (extreme rare period) 3.3. Vertebral shaping and bone shaping. The goals of vertebroplasty and arthroplasty: The goals of vertebroplasty and spondyloplasty are to relieve pain and improve mobility in disabled patients with vertebral fractures. Spine reshaping can also help restore part or all of the bone's height and, therefore, improve the alignment of the spine.
Most commonly, these procedures are used to treat compression fractures caused by osteoporosis. Less commonly, the procedure is used to treat fractures caused by cancer, trauma, or bone necrosis. Doctors said:
How to prepare for vertebroplasty: If the patient decides to have vertebroplasty or spondyloplasty, the doctor will provide many instructions before surgery.
These instructions may include:
Stop taking certain medications one week before the procedure (eg, nonsteroidal anti-inflammatory drugs, NSAIDs, or blood thinners). Stop eating six hours before surgery. Arrange for someone to drive the patient home after surgery. Preparation for the day of surgery: With both angioplasty and spondyloplasty, bone cement is injected into the broken vertebra. Kyphoplasty also involves creating a cavity with a special ball.
For kyphoplasty, the patient can take the following steps on the day of surgery:
On arrival, the patient will change into a hospital gown and the nurse will insert an IV tube. The patient will be taken to the operating room and will lie face down on the table. The anesthesiologist will give the patient medicine to put the patient to sleep. The surgeon will make a small incision (cut) over the area of the broken vertebra. Using X-ray guidance, the surgeon inserts a special instrument called a trocar (a needle surrounded by a narrow tube) into one side of the broken vertebra. A special balloon is passed through the trocar and inflated to create an opening inside the bone. When the new cavity is created, the balloon is deflated and removed. The surgeon will inject bone cement into the cavity and close the incision. The patient will continue to lie on the operating table until the cement hardens (this takes a few minutes). After the procedure takes less than an hour, the patient will be taken to the recovery room. When the anesthetic wears off, most patients can go home the same day.
Recovery: Some patients will experience immediate pain relief after spondylolisthesis or spondyloplasty. But for others, the pain relief subsides within a few days.
Before the patient leaves the surgical center, the doctor will give the patient various instructions, such as:
Apply ice to the back (if needed) for pain related to the procedure. Return to normal activities (usually immediately) and avoid strenuous activities for a period of time (usually six weeks) Follow up with your doctor to manage osteoporosis (if that's the cause) behind the patient's vertebral fracture). Long-term care of patients: Vertebral fractures are common, especially in the elderly, post-menopausal women, in which osteoporosis is common. Because of the potentially disabling severe pain associated with these fractures, it makes sense in the long run to prevent another fracture from occurring.
Prevention of osteoporosis-related vertebral fractures requires participation in various non-pharmacological therapies.
These therapies include:
Perform weight-bearing exercises daily Ensure adequate calcium intake and vitamin D supplementation Stop smoking Moderate alcohol intake Address strategies to prevent falls (eg: avoid high-risk medications, correct vision problems, etc.) In some cases, medications for osteoporosis, such as bisphosphonates, may be prescribed.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: vi1.m-almahdi.com