This is an automatically translated article.
When the life span of red blood cells is shortened because the body produces autoantibodies against red blood cells and this is the main cause of autoimmune hemolytic disease. Red blood cells are destroyed either by phagocytosis that occurs in the endothelial system or by activation of the complement system that causes red blood cell lysis.
1. What is autoimmune hemolytic disease?
Autoimmune hemolysis is anemia caused by the body not having enough red blood cells. Red blood cells in the body are broken down earlier than normal by the appearance of anti-erythrocytic autoantibodies.
The role of red blood cells is to help carry oxygen throughout the body. Each red blood cell lasts in the body from 100 - 120 days, however, in case the immune system in the body is disturbed and mistakenly recognizes red blood cells with foreign antigens, it should be removed from the body. That produces antibodies that destroy red blood cells, causing them to die earlier than normal. If autoimmune hemolysis is severe, the life cycle of red blood cells is only a few days.
Autoimmune hemolytic disease can develop rapidly or progress gradually over time.
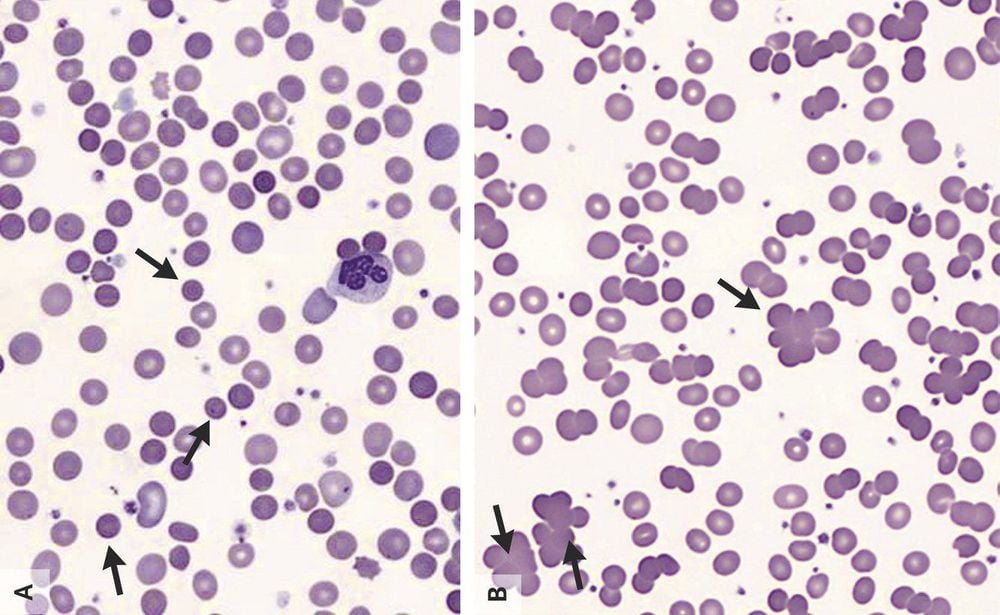
Hình ảnh hồng cầu bị phá vỡ
2. Mechanism of autoimmune hemolysis
Blood cells are made in the bone marrow and are classified into 3 basic types of blood cells as follows:
White blood cells : They are responsible for helping the body fight infections; Platelets: Have the task of participating in blood clotting and preventing prolonged bleeding; Red blood cells: Responsible for transporting oxygen throughout the body in the form of hemoglobin. With the task of helping the body fight infections, white blood cells will produce antibodies. These antibodies are then attached to red blood cells and travel throughout the body, fighting germs and foreign particles that need to be eliminated.
In patients with autoimmune hemolytic disease, the immune system is disordered, antibodies produced by white blood cells recognize red blood cells containing foreign antigens and need to be removed. Consequences of the formation of abnormal antibodies against antigens present on the patient's red blood cells, usually IgG and IgM antibodies, bind complement, thereby causing erythrocyte rupture.
RBC rupture is divided into 2 types:
Intravascular (intravascular) red blood cell rupture is an antigen - antibody - complement reaction on the surface of red blood cells by IgG or IgM; The phenomenon of rupture of extravascular red blood cells (in the inter-retinal organization: liver, spleen, extravascular ...) by phagocytosis, they eat antibody-bound red blood cells.
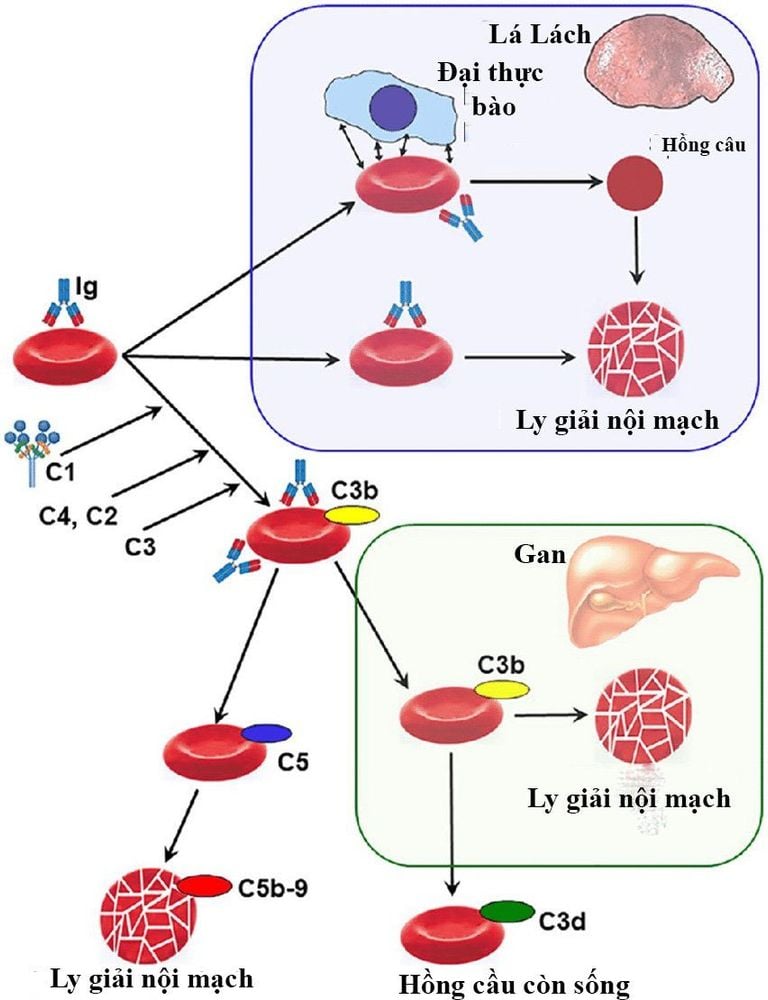
Hình ảnh mô tả cơ chế gây tan máu tự miễn
Exposure to certain toxins or chemicals, such as complications from taking anti-infectives; Received blood transfusion but the blood group is not suitable; The fetal blood group is different from the mother's blood type; Certain types of cancer.
3. Classification of autoimmune hemolytic diseases
Autoimmune hemolytic anemia occurs in the presence of anti-erythrocyte antibodies. Anti-erythrocytic antibodies are classified as follows:
Anti-erythrocytic antibodies work at a temperature of 37 degrees Celsius - normal body temperature (hot antibodies): This class is related to IgG antibodies . Autoimmune hemolysis due to hot antibodies accounts for over 80-90% of cases; Anti-erythrocytic antibodies that work at temperatures below 37 degrees Celsius (cold antibodies): This involves “cold” IgM or agglutinin antibodies, which bind to red blood cells when the blood is exposed to heat cold (about 0 - 4 degrees Celsius). This type of autoimmune hemolysis accounts for only about 10-20% of cases. In addition, autoimmune hemolytic disease is also classified according to primary and secondary causes:
Primary (idiopathic): A disease condition that occurs when there is no other health problem causing; Secondary cause: This is when the condition is associated with another health condition such as Rheumatoid Arthritis, Systemic Lupus Erythema (SLE), Sjogren's Syndrome, Colitis, Hashimoto's Thyroiditis, Kidney Disease Prolonged, Other problems weaken the immune system.
Viêm đại tràng có thể là nguyên nhân thứ phát gây bệnh tan máu tự miễn
4. Symptoms of disease
Autoimmune hemolysis causes anemia very quickly which can be life threatening. Need to quickly go to reputable medical facilities if the body shows the following symptoms:
Mild fever; Fatigue, weakness; Difficulty concentrating and thinking; Haggard; heart palpitations; Shortness of breath; Jaundice ; Dark urine; Nausea, vomiting and diarrhea; Dizziness when standing up; Tongue pain.

Bệnh tan máu tự miễn có thể gây khó thở
Customers who need medical examination and treatment can directly go to Vinmec Health System nationwide or contact the hotline HERE for support.
MORE:
What is an autoimmune disease? How is thalassemia (congenital hemolysis) detected? How is thalassemia (congenital hemolysis) treated?