This is an automatically translated article.
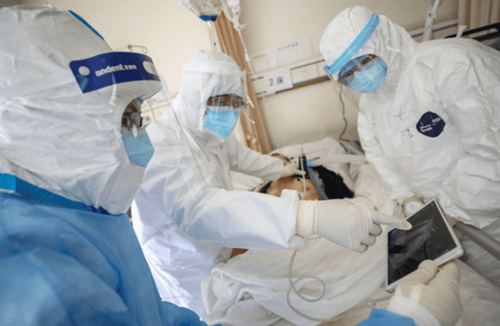
Ventilators have become a symbol during the COVID-19 pandemic, the last hope for survival in patients who cannot breathe on their own. However, when they need a ventilator, their condition is in the most serious stage.
1. Delay the use of ventilators for patients
Around the world, many COVID-19 patients, despite being on ventilators, still did not survive. At the same time, people who are currently battling COVID-19 will likely face respiratory problems caused by both the machine and the corona virus. The problem is, the longer people are on a ventilator, the more likely they are to experience complications related to this assistive device.
Realizing this, some intensive care units in New York City hospitals have begun to delay the use of ventilators. The pulmonologists here only use ventilators for COVID-19 patients when it is really the final decision regarding life, when they have no other choice or cannot extend it any longer.
Early in the COVID-19 crisis, there was a tendency to put patients on ventilators early when their condition was rapidly deteriorating. For now, doctors let these patients suffer a little more. They give the patient some oxygen but do not intubate until the patient is truly in respiratory failure. Ventilators need to be ordered at the correct time, no earlier than before the patient needs it, and when that is the only option.
2. Priority criteria for using ventilators for COVID-19 patients

Trường hợp nhiễm COVID-19 nặng dù có sử dụng máy thở cũng tử vong thì sẽ không được sủ dụng
During the COVID-19 pandemic, ventilators become more scarce, many hospitals in New York and European countries are facing shortages of ventilators and ICU beds. The problem has become urgent when doctors here have to decide which patients should be placed on ventilators in overcrowded conditions. Hospitals all emphasize respect for patients and families, fairness and transparency. That means the patient is told exactly which cases will be prioritized to use the ventilator. Some general principles include:
Provide ventilators to people who really need them. That is, the person who is most at risk of death if not on a ventilator, and most likely to survive if breathing is given; If the patient is clearly going to die, even with a ventilator, that will not be a priority. For example, people at high risk of dying in a short time, including those with advanced cancer or Alzheimer's; Decisions are not based on first-come, first-served basis or random selection, but will use a rating scale to assess the function of agencies. For example, people with severe kidney, pancreatic, or other organ disease, or who are already in a coma, will not be given priority to use a ventilator; The first priority is not for the person who pays for it, has any insurance coverage, rich or poor, ethnicity, race or gender. However, certain target groups, such as healthcare professionals, may be preferred; Young people are generally more privileged than older people; There is no discrimination against people with disabilities. If the patient has an intellectual disability, or is confined to a wheelchair, but the organs are still functioning well, priority is still given.
3. Critically ill patients still die even with ventilators
Hình ảnh bệnh nhân nguy kịch vẫn tử vong dù có máy thở
Experts estimate that about 40 - 50% of patients still die after mechanical ventilation, regardless of their underlying disease. Currently, it is too early to draw conclusions for COVID-19 patients, but some areas in New York have reported that up to 80% of people infected with the virus die after being on ventilators.
On the other hand, there is an opinion that critically ill patients die because of the devastation of the COVID-19 virus, not because the ventilator seriously harms them. The majority of deaths are not related to the ventilator. Critically ill patients still die with or without mechanical ventilation.
Last month, a patient in critical condition in New York City was on a ventilator 6 days after being diagnosed with COVID-19. When he was hospitalized, a doctor warned him that it was best not to put on a ventilator, because many people did not survive after using this device.
This patient is now alive and grateful for the ventilator, but he is also trying to restore his ability to breathe on his own. He said he felt short of breath even with mild exertion. Although he used to run a marathon in the past, he now can't walk through the next room or up the stairs because he can't breathe. The patient is also unable to get around to get fresh air unless pushed by a loved one in a wheelchair.
4. Complications of ventilators

Máy thở không xâm lấn là một trong các loại máy thường được sử dụng điều trị cho bệnh nhân
Types of ventilators commonly used are non-invasive ventilators, CPAP continuous positive pressure ventilators,... In which, continuous positive pressure machines, English name is Continuous Positive Pressure Ventilation (CPPV), Both inspiratory and expiratory pressures are positive thanks to a valve that prevents exhalation called PEEP (Positive End Expiratory Pressure). CPAP ventilator is a way of natural ventilation, which stands for Continuous Positive Airway Pressure, to improve the mechanical factors of the lungs and improve gas exchange.
In general, ventilators still carry the risk of a wide range of side effects. These complications, combined with lung damage from COVID-19, can make recovery difficult and long.
The ventilator pushes air into the patient's lungs, they must be sedated and an endotracheal tube inserted in the throat. Because of mechanical ventilation, the patient's diaphragm and all other muscles involved in breathing will be weakened. When all of these muscles become weaker, the patient will have difficulty breathing even though the condition has been reached and weaned off the ventilator.
Patients are also at risk for ventilator-associated acute lung injury. This condition occurs as a result of pulmonary embolism due to improper ventilatory care. Doctors must calculate exactly how much air to push into each person's lungs. In fact, most of the lungs can be filled with fluid and are unable to take in too much oxygen, so the amount of air needed will often be less than it needs. If the readings are not set correctly, the ventilator will cause further injury to the lungs.
Ventilator patients are also at high risk of infection. Even many people have psychological complications. According to doctors, a quarter of patients develop post-traumatic stress disorder, and up to 50% of people develop depression afterward. The longer you stay on the ventilator, the more likely these complications are.
That's why ICUs (intensive care) are gradually becoming more cautious in using ventilators. They prefer to use oxygen and breathing relaxants, like nitric oxide, to keep people exhaling on their own for as long as possible. The ventilators are not drugs, they only help the body to deal with the inflammation caused by the infection. Patients cannot be expected to improve the next day if they are placed on a ventilator.
To register for examination and treatment at Vinmec International General Hospital, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.













