This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Patients with inflammatory bowel disease (IBD) can develop complications from the disease itself and also from the immunosuppressive therapies used to treat it. To optimize care for patients with IBD, clinicians need to consider primary, secondary, and tertiary prevention. Primary prevention is used to prevent disease or complications from developing, such as vaccination. This review highlights prevention methods that can be used in patients with IBD through a partnership between the primary care provider and the gastroenterology department.
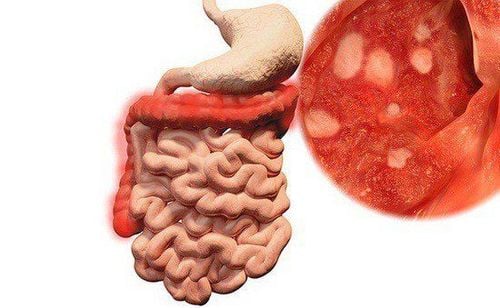
1. Overview of inflammatory bowel disease
Inflammatory bowel disease (IBD), including Crohn's disease (CD) and ulcerative colitis (UC), causes inflammation and ulceration of the gastrointestinal tract. This inflammation leads to significant morbidity for the patient, including symptoms such as diarrhea, abdominal pain, rectal bleeding, and weight loss. Rates of IBD are increasing in the United States (US) and around the world. It is estimated that 2.2 million Americans will live with IBD by 2025. With the population growing, there is a growing need for safe and effective therapies to control inflammation.
Currently, there are a large number of drugs for the treatment of IBD, with varying relationships between safety and effectiveness. Immunosuppressive agents used in the treatment of IBD include corticosteroids, anti-tumor necrosis factor alpha (anti-TNF) biologic agents, anti-tumor therapies, and anti-IL-12/antibody inhibitors. 23, janus kinase (JAK) inhibitors and immunomodulators such as thiopurine methotrexate. Since the authors targeted mucosal healing in their IBD population using immunosuppressants, they also had to use a patient-centered approach to prevent complications. later, of IBD itself or of the therapies used to treat IBD. To do so, collaboration between gastroenterologists and other specialists is required to target primary, secondary, and tertiary prevention for patients.
2. Primary prevention
Primary prevention is defined as preventing the development of disease. Examples of primary prevention efforts include immunization against infectious diseases or educational interventions about regular exercise.
Initial prevention efforts can occur at the individual or population level. An example of a population-level primary prevention effort is fluoridation of water supplies to prevent tooth decay. Compared with the general population by age, IBD patients are at increased risk for vaccine-preventable diseases, such as influenza, pneumococcal pneumonia, and shingles. The inactivated vaccine is safe to use in IBD patients, regardless of immunosuppressive status.
Therefore, following immunization guidelines for inactivated vaccines can reduce these infectious complications. Annual influenza vaccine is indicated in all IBD patients, pneumococcal vaccine is indicated in all immunosuppressed patients with IBD, and herpes zoster vaccine is indicated in all IBD patients 50 years of age .
Because of the increased risk of shingles in the younger IBD population, earlier vaccination may be considered when some high-risk patients are being treated. In particular, tofacitinib has been associated with an increased risk of shingles, especially at higher doses. However, more data on safety, efficacy, and durability in younger populations are needed before formal recommendations can be made.
The humanpapillomavirus (HPV) vaccine has been shown to protect against specific serotypes of HPV that are associated with cervical dysplasia and genital warts. This vaccine has been studied specifically in IBD populations. The HPV vaccine has proven both effective and safe.

3. Preventing Skin Cancer in IBD Patients
Another major prevention method in IBD patients is the use of sunscreen to prevent skin cancer. IBD patients have an increased risk of both non-melanoma skin cancer (NMSC) and melanoma skin cancer. Evidence has demonstrated that thiopurines specifically increase the risk of NMSC and that the mechanism of action is related to photosensitivity to ultraviolet-A. It is therefore a preventable complication of therapy through the use of broad-spectrum sunscreens. Finally, weight-bearing exercise and calcium/vitamin D supplementation, when appropriate, may prevent downstream osteoporotic fractures in these patients, who may require repeated courses of corticosteroid therapy. develop during the time they have IBD.
All age-appropriate vaccines should be given
In addition to what is highlighted, people with IBD should get all age-appropriate vaccines, except live vaccines. should be avoided in patients on immunosuppressive therapy.
Immunosuppression is defined as continuous use of corticosteroids, biologic agents (anti-tumor necrosis factor alpha, anti-integrase, anti-IL 12/23), immunomodulatory drugs (azathioprine or methotrexate) or small molecules (tofacitinib)
4. Secondary prevention
Secondary prevention is defined as early disease detection to prevent disability; such as through screening programs. Therefore, there are some important opportunities for secondary prevention in IBD patients. For example, patients with IBD are known to have an increased risk of melanoma, regardless of immunosuppressive therapy. Individuals taking anti-tumor necrosis factor alpha (anti-TNF) drugs have a nearly twofold increased risk of developing melanoma. Therefore, a dermatological examination program is recommended in all patients with IBD. Previous studies have suggested an increased risk of abnormal cervical smear and/or cervical dysplasia in immunosuppressed IBD patients.
Cervical cancer screening in female patients with IBD
Therefore, annual cervical cancer screening is recommended in immunosuppressed IBD patients. IBD patients with perennial colitis (lasting >10 years) are at increased risk for colorectal dysplasia and cancer. Therefore, patients with long-standing colitis should undergo periodic colonoscopy starting at 8-10 years of colonic disease, with subsequent colonoscopy intervals based on findings (usually 1- 1 year). every 3 years).
Osteoporosis risk assessment
From a bone health perspective, all individuals (regardless of sex) with a duration of ≥ 3 months of corticosteroid use are at risk for developing osteoporosis or osteoporosis. Therefore, screening with a DEXA scan is recommended for these individuals and in women over 65 years of age. Subsequent DEXA screening may be determined based on initial results. Finally, depression and anxiety are common in IBD patients. Early recognition and treatment of depression and anxiety can improve quality of life in patients with IBD. All patients with IBD should be screened for depression and anxiety.

5. Tertiary prevention
Tertiary prevention refers to the use of measures to reduce the impact of long-term illness and disability. In Crohn's disease, ongoing inflammation can lead to the development of narrow slits, which can cause blockages and require surgical resection of the bowel. Additionally, inflammation can progress to leaky gut disease, which involves abnormal connections between the intestines and other organs. These fistulas can lead to abscesses and other complications that often require surgery.
In ulcerative colitis, ongoing inflammation can increase the risk of colon cancer and dysplasia. In addition, the disease may extend from involving only the left side to involving the colon over time. Thus, by early intervention and treatment of inflammation, with the goal of mucosal healing, we can prevent the morbidity and potentially life-threatening complications of IBD. The IBD management model has shifted to one of the “treat with the goal” approach.
6. Re-evaluate after treatment for inflammatory bowel disease
After initiating medical therapy for IBD, guidelines recommend subsequent reevaluation to ensure that both symptoms and mucositis improve. This dual reevaluation approach is important, as symptoms do not always correlate with ongoing inflammation. This current standard of reevaluation of therapy is also important in postoperative CD, where early endoscopic evaluation is in the first 6-12 months after resection, with alteration of medical therapies based on this. , has been shown to improve long-term endoscopy. results Thus, by optimizing therapies to improve mucosal healing, we were able to impact the long-term disability associated with irreversible bowel damage in IBD.
Conclusion
The management of patients with IBD can be difficult. IBD itself may be associated with a number of complications for patients, including ongoing chronic bowel symptoms and structural damage to the gut, as well as extraintestinal manifestations of IBD. These extraintestinal manifestations can include severe joint symptoms, skin manifestations, anemia, and kidney stones. While there are a number of effective treatments for treating IBD and these extraintestinal complications, many of these therapies are self-immunosuppressive. Therefore, the drug itself can cause treatment-related complications. These may include infectious, malignant, or idiopathic complications. When a patient is able to present to a primary care provider or a gastroenterologist to evaluate symptoms or complications, it becomes very important for the entire care team to collaborate. in the diagnosis and management plans for each patient with IBD. Every IBD patient should be evaluated regularly with both a primary care physician and a gastroenterologist. Through this partnership, an individual preventive health plan can be developed for each patient with IBD. This proactive approach to addressing primary, secondary, and tertiary prevention in IBD patients can ultimately help reduce transmission.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, inflammatory bowel disease, short bowel syndrome, diseases causing chronic diarrhea , Crohn's disease, ectopic gastric mucosa in the esophagus...
Vinmec Hospital with modern facilities and equipment and a team of experienced experts, always dedicated to medical examination and treatment, Customers can rest assured with gastroscopy and esophagoscopy services at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol 2015;12:720-7. Kaplan GG, Ng SC. Understanding and Preventing the Global Increase of Inflammatory Bowel Disease. Gastroenterology 2017;152:313-321.e2. Fararraye FA, Melmed GY, Lichtenstein GR, et al. ACG Clinical Guideline: Preventive Care in Inflammatory Bowel Disease. Am J Gastroenterol 2017;112:241-258. 4. Uma Mahadevan MD, Prevention in Inflammatory Bowel Disease: An Updated Review, Practice Enterology