This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Today, an accurate diagnosis of inflammatory bowel disease is an increasingly important issue, helping doctors understand the condition, and get effective treatment right from the start.
1. Overview of inflammatory bowel disease
Inflammatory bowel disease (IBD) is a chronic and idiopathic inflammatory disease of the gastrointestinal tract that shows an episode of remission and recurrence. Ulcerative colitis (UC) and Crohn's disease (CD) are the two main forms of inflammatory bowel disease. The number of IBD patients has increased rapidly in recent years and is increasingly prominent in Korea. However, many physicians still do not fully understand the clinical and endoscopic features of inflammatory bowel disease, so diagnosis is often delayed or inaccurate in many cases. Accurate diagnosis of inflammatory bowel disease is an increasingly important issue. The diagnostic guideline for inflammatory bowel disease was established by the Inflammatory Bowel Disease Research Group of the Korean Intestinal Diseases Research Association in 2009. In this article, we describe typical endoscopic findings and features The differential diagnosis of UC, CD, inflammatory bowel disease, and intestinal tuberculosis is based on these guidelines.
2. Typical endoscopic signs of inflammatory bowel disease IBD
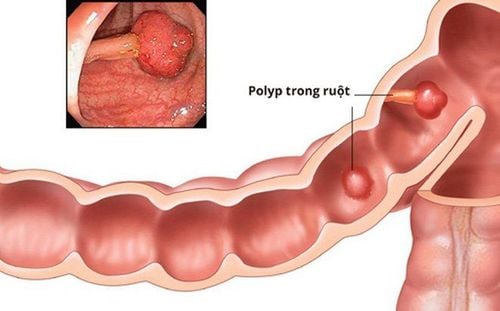
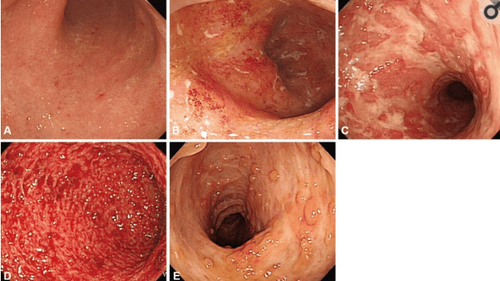
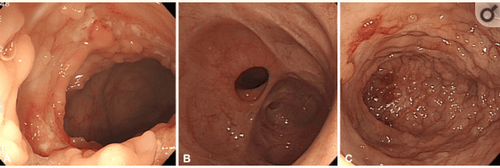
2.1 Ulcerative Colitis Inflammation involving the rectum in most cases and spreading to the surrounding area. Typical endoscopic findings in patients with ulcerative colitis include mucosal edema, congestion, loss of vascular structure, and mucosal sclerosis. More severe cases may result in erosions, ulcers, and spontaneous bleeding. Intestinal stenosis and pseudomembranous formation can occur due to chronic inflammation, leading to mucosal atrophy. Localized inflammation around the orifice of the appendix is observed in 75% of patients with ulcerative colitis.
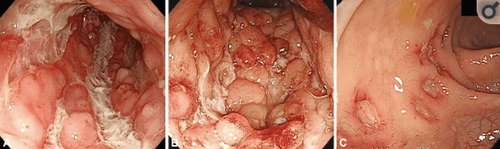
2.2 Crohn's Disease Typical endoscopic findings in Crohn's include a discontinuous distribution of longitudinal ulcers (defined as ulcers ≥4 to 5 cm by Japanese standards), protrusion appearance of cobblestones and/or longitudinally arranged asteroid ulcers. A Korean study reported that 37.2% had longitudinal ulcers, 23.9% had stones, and 59.3% of newly diagnosed Crohn's cases. Granulomatous imaging, a biopsy feature suggestive of Crohn's, may be seen in only 13% to 36% of patients with Crohn's, thus the sensitivity of biopsy is low.
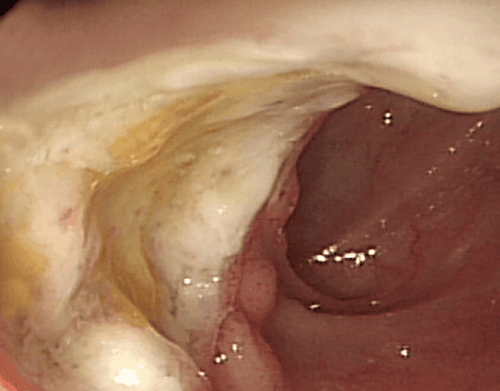
Esophageal endoscopy is not routinely recommended in patients with Crohn's disease unless upper gastrointestinal symptoms are present. Gastroduodenal Crohn's disease presents with nonspecific lesions such as erosive, congestive, or ulcerative. A bamboo joint-like appearance can be seen on endoscopy, which is characterized by longitudinal folds, swelling through erosive fissures or linear grooves on the lesser curvature of the gastric body and gastric cardia. .
2.3 Intestinal Tuberculosis Tuberculosis of the bowel usually involves the ileum and ascending colon. Endoscopic findings of intestinal tuberculosis may include transverse ulcers, nodules with inflammatory changes of the surrounding mucosa, pseudomembranous, and/or deformed ileal valves and lumen narrowing. Although the typical histologic features of case granulomas, positive acid-fast staining, and/or isolation of Mycobacterium tuberculosis from biopsy specimen culture can confirm intestinal tuberculosis, these findings are present in few more than 50% of patients. Therefore, more than three biopsies should be obtained from the margin and base of the ulcer to increase diagnostic yield.
3. Differential diagnosis of inflammatory bowel disease
3.1 Ulcerative colitis and other causes of enteritis The differential diagnosis of ulcerative colitis includes infectious colitis, ischemic colitis, drug-induced colitis, and inflammatory colitis. radiation and isolated rectal ulcer syndrome. Previous history of abdominal pain, medication, radiation therapy, or straining to defecate may be helpful.
Clinicians should always keep in mind that there are no specific endoscopic findings for ulcerative colitis. Infectious colitis may present with endoscopic features similar to those of ulcerative colitis. Therefore, for an accurate diagnosis, the onset and duration of symptoms should be considered together. Microbial cultures may also be helpful to distinguish ulcerative colitis from infectious colitis. Indeed, in a multinational web-based survey conducted by the Asia Foundation on Crohn's Disease and Colitis, more than half of Asian gastroenterologists reported always or frequently performing cultures. microbiology for ulcerative colitis.
3.2 Ulcerative Colitis and Crohn's Disease Ulcerative colitis mainly presents with proctitis and continuous lesions, while Crohn's disease presents with intermittent inflammatory lesions usually involving the ileum region. Shallow and non-discursive ulcers involving only the mucosa, with edematous and congestive changes in the surrounding area may suggest ulcerative colitis. Crohn's disease can involve not only the colon but also the small intestine, and often present with deep ulcers. The ulcers are deep, with longitudinal plaque forming stones. The rectum is sparse, there is perianal disease, and the presence of cuts and fistulas suggest Crohn's disease.
Use of serologic markers can help differentiate UC and Crohn's. Anti-Saccharomyces cerevisiae (ASCA) antibodies can be detected in 35% to 50% of patients with Crohn's disease, but only in 1% of patients with ulcerative colitis. On the other hand, anti-paranuclear cytoplasmic antibodies (pANCA) were detected more frequently in patients with ulcerative colitis. The sensitivity of pANCA+ for ulcerative colitis was reported to be 55.3%, and ASCA+ combined with pANCA– resulted in a sensitivity of 54.6% for the detection of Crohn's. Given the relatively low sensitivity, serologic testing can be an adjunct when clinically difficult to differentiate between Crohn's disease and ulcerative colitis.
Table 1.
Differential diagnosis of ulcerative colitis and Crohn's disease
| Đặc tính | Viêm loét đại tràng | Bệnh Crohn |
| Tổn thương ở trực tràng | Gần như luôn luôn | Thường xuyên |
| Tổn thương ở ruột non | Rất hiếm | Thường xuyên |
| Tổn thương liên tục | Luôn luôn | Không thường xuyên |
| Độ sâu của vết loét | Niêm mạc | Sâu hơn niêm mạc |
| Hình ảnh đá cuội | Không | Có |
| Hẹp lòng ruột | Rất hiếm | Thường xuyên |
| Lỗ rò | Không | Thường xuyên |
| Tổn thương quanh hậu môn | Không | Thường xuyên |
| pANCA | ++ | + |
| ASCA | + | ++ |
In which: UC, ulcerative colitis; CD, Crohn's disease; pANCA, anti-paranuclear cytoplasmic antibody; ASCA, anti-Saccharomyces cerevisiae antibody.
3.3 Crohn's Disease and Intestinal Tuberculosis The presence of longitudinal ulcers is a typical endoscopic finding in Crohn's disease, whereas transverse ulcers are common in intestinal tuberculosis. However, because these typical findings are not always present, it is often difficult to distinguish between the two diseases. In a Korean study evaluating the diagnostic value of various endoscopic findings in Crohn's disease and intestinal tuberculosis, anorectal lesions, longitudinal ulcers, aphthous ulcers, and cobblestone appearance were observed. are frequent in Crohn's disease, whereas involvement of less than 4 segments, a severe ileal valve, transverse ulceration, and scarring or pseudo-scarring are commonly seen in intestinal tuberculosis. Using these parameters, an accurate diagnosis was made in 87.5% of patients, with a positive predictive value of 94.9% for Crohn's disease and 88.9% for intestinal tuberculosis, respectively. . However, this analytical method has not yet been validated and further studies are needed.
Table 2
Endoscopic features of Crohn's disease and intestinal tuberculosis
| Đặc tính | Bệnh Crohn | Bệnh lao ruột |
| Có tổn thương van hồi manh tràng | Phổ biến | Thường có, gây hẹp van hồi manh tràng |
| Có tổn thương đại tràng | ≥4 đoạn, đặc biệt là đoạn cuối hồi tràng và van hồi manh tràng | <4 Phân đoạn, đặc biệt là van hồi manh tràng và đại tràng xuống |
| Loét | Theo chiều dọc | Ngang |
| Hình ảnh đá cuội | Thường xuyên | Hiếm |
| Tổn thương xung huyết | Thường xuyên | Hiếm |
| Tổn thương quanh hậu môn | Thường xuyên | Hiếm |
| Sẹo / giả mạc | + | ++ |
In which: CD: Crohn's disease; ITB: intestinal tuberculosis; ICV: ileocecal valve
Typical histologic findings of granulomas and positive acid-fast staining are seen in less than 30% of patients with intestinal tuberculosis, but chest x-ray and interferon-γ testing can assist aid in the diagnosis of intestinal tuberculosis. In fact, 67% of patients with intestinal tuberculosis had active pulmonary TB in a Korean study. Therefore, chest x-ray is an essential test in intestinal tuberculosis. The Interferon-γ test may also be useful as an additional diagnostic tool for intestinal tuberculosis. A recent Korean study reported that 66% of patients with intestinal tuberculosis had a positive interferon-γ test (QuantiFERON-TB Gold test), compared with 9.7% of patients with crohn's disease.
If the exact diagnosis of the two diseases is still unclear despite the above methods, it may be helpful to perform a follow-up colonoscopy after empiric anti-tuberculosis therapy.
3.4 Crohn's disease (CD) and intestinal Behcet's disease (BD) A Korean study proposed an algorithm for differential diagnosis of CD and intestinal Behcet's disease according to endoscopic features. Ulcer shape, distribution, number, margin and border of lesions, and presence of aphthous, cobblestone, perianal, and tight lesions allow an accurate diagnosis of Behcet's disease or CD. intestine in 92% of the study population. Among these parameters, the most sensitive detectable sign of intestinal BD was the absence of gallstones and most notably the round ulceration. In addition, the distribution pattern in patients with intestinal Behcet disease was more concentrated than in patients with CD. Therefore, a circular ulcer or clustered lesions in the intestinal tract may suggest Behcet's disease of the intestine.
Another Korean study proposed simple criteria for the diagnosis of intestinal Behcet's disease using systemic and endoscopic features. 5 or less lesions, oval, deep infiltrates, discrete boundaries, and ileal sites are considered typical ulcers in Behcet's disease. Overall, the positive predictive value and diagnostic accuracy using these criteria were 86.1% and 91.1%, respectively.
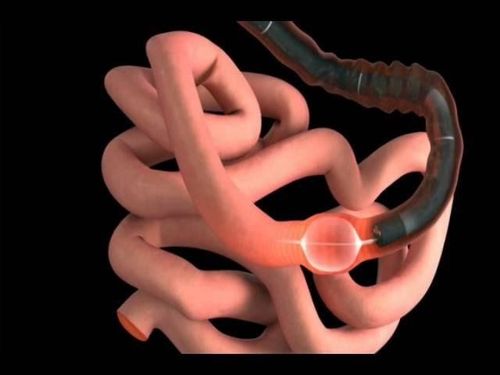
In summary, colonoscopy is the primary test for the diagnosis of inflammatory bowel disease. Clinicians can accurately diagnose most cases by fully understanding typical endoscopic findings. However, in some cases, it is difficult to differentiate inflammatory bowel disease because of its atypical presentation. Therefore, not only endoscopic features but also clinical symptoms, as well as laboratory, pathological, and radiological findings should be considered.
At Vinmec International General Hospital, the diagnosis through colonoscopy with Olympus CV 190 endoscope, with NBI function (Narrow Banding Imaging - endoscopy with narrow light frequency band) gives results. Mucosal pathology analysis images are clearer than conventional endoscopy, detecting ulcerative lesions in the colon. Not only the physical system, modern equipment: 6 ultrasound rooms, 4 DR X-ray rooms (1 full-axis machine, 1 light machine, 1 general machine and 1 mammography machine) , 2 DR portable X-ray machines, 2 multi-row computer tomography rooms with receivers (1 machine 128 rows and 1 machine 16 rows), 2 rooms for magnetic resonance imaging (1 machine 3 Tesla and 1 machine 1.5 Tesla), 1 room for 2 level interventional angiography and 1 room for bone mineral density.... Vinmec is also the place to gather a team of experienced doctors and nurses who will greatly assist in the diagnosis and detection. early signs of abnormality of the patient's body. In particular, with the space designed according to hotel standards, Vinmec ensures to bring the patient the most comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008;14:542–549. [PubMed] [Google Scholar] Suzuki Kurokawa M, Suzuki N. Behcet's disease. Clin Exp Med. 2004;4:10–20. [PubMed] [Google Scholar] Kim YS, Kim YH, Lee KM, Kim JS, Park YS, IBD Study Group of the Korean Association of the Study of Intestinal Diseases Diagnostic guideline of intestinal tuberculosis. Korean J Gastroenterol. 2009;53:177–186. [PubMed] [Google Scholar] Choi CH, Jung SA, Lee BI, et al. Diagnostic guideline of ulcerative colitis. Korean J Gastroenterol. 2009;53:145–160. [PubMed] [Google Scholar] Ye BD, Jang BI, Jeen YT, et al. Diagnostic guideline of Crohn's disease. Korean J Gastroenterol. 2009;53:161–176. [PubMed] [Google Scholar] Ji Min Lee and Kang-Moon Lee, Endoscopic Diagnosis and Differentiation of Inflammatory Bowel Disease, Clin Endosc. 2016 Jul; 49(4): 370–375. [PubMed] [Google Scholar]