This is an automatically translated article.
Article by Doctor Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International Hospital.According to the World Health Organization (WHO), seven countries account for 64% of TB cases in the world: India, China, Indonesia, Philippines, Pakistan, Nigeria, and South Africa; This distribution of tuberculosis closely reflects the distribution of poverty, malnutrition and low income.
1.Risk factors for pulmonary tuberculosis
Risk factors for acquired pulmonary TB include malnutrition, HIV (human immunodeficiency virus) infection, parenteral drug use, diabetes mellitus, prolonged use of corticosteroids, chronic renal failure / extrarenal dialysis, silicosis, solid organ transplantation, and carcinoma of the head and neck.
Risk factors for CNS TB include malnutrition, alcoholism, co-morbid malignancies, use of immunosuppressive drugs, HIV infection, recent measles infection, and disease measles in children.
Studies in developed countries have also determined that people born outside of developed countries account for a higher than expected proportion of CNS TB cases.
Although CNS TB is most commonly seen as a complication of pulmonary TB, imaging of the lungs may show inactive TB infection; CNS TB is not uncommon in people who have been treated for pulmonary tuberculosis years or even decades ago.

Although there have been advances in our understanding of the pathogenesis and treatment of CNS TB over the past 50 years, the emergence of MDR-TB and MDR-TB, the Acquired immunodeficiency (AIDS) and subsequent access to highly potent antiretroviral therapy that can induce the inflammatory immune remodeling syndrome further complicate diagnosis and management. Central nervous system tuberculosis treatment.
Advances in diagnostic tests promise to increase the speed of diagnosis as well as the percentage of people who have a confirmed diagnosis rather than a presumptive diagnosis. Advances in precision medicine have identified polymorphisms in the LTA4H gene that influence the risk of inflammation in patients with tuberculous meningitis.
The most common clinical form of central nervous system tuberculosis is tuberculous meningitis, which is most common in young children (especially children under 1 year of age); At presentation, 75% of children have active pulmonary TB, and tuberculous meningitis is most common within 3 months of primary infection. Rich and McCordock initially hypothesized that tuberculous meningitis originates from the spread of infection into the subarachnoid space from a tubercle necrosis proximal to the cerebral cortex (Rich's foci).
A later hypothesis agrees with this but also suggests that initial hematogenous dissemination may cause a tubercle of tuberculoma in the meninges or cerebral cortex followed by tuberculous meningitis. or some time later. One reinforcement of this route of transmission was observed in a man who attempted suicide by injecting live tubercle bacilli into an anterior forearm vein and developed tuberculous meningitis 86 days later.
2. Manifestations of tuberculous meningitis
The neurological manifestations of tuberculous meningitis may be insidious or abrupt, resembling bacterial or viral meningitis. The most common symptoms of tuberculous meningitis include fever, vomiting, and lethargy. Because there is often damage to the base of the skull and surrounding cisterns in tuberculous meningitis, cranial nerve dysfunction is common, with cranial nerves VI (abdomen), VII (facial), and II (optical nerves). senses) are most commonly affected.
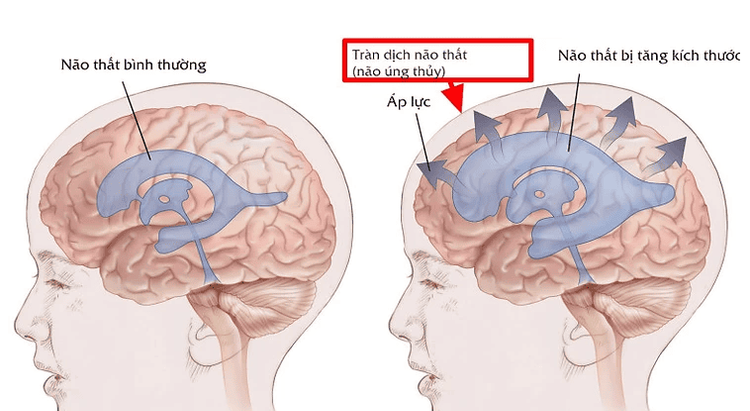
On neuroimaging, a common triad of findings includes increased basal meningeal enhancement, hydrocephalus, and foci of infarction in the supratenta and brainstem parenchyma. The case below illustrates a typical profile of a patient with tuberculous meningitis.
Hydrocephalus is a common complication of tuberculous meningitis. When cerebrospinal fluid (CSF) protein is elevated above 500 mg/dL, cerebrospinal fluid obstruction can occur and cause subarachnoid occlusion, leading to hydrocephalus. Obstruction is most common in the tentorial aperture pools when the septum passing through this space is obstructed by fibrin deposition, causing hydrocephalus which can lead to pseudohypertension and loss of normal response. open pressure is often increased during jugular venous compression.
3.Example of clinical cases
A 17-year-old male patient presents to the emergency department with 2-week history of headache, nausea, and vomiting. Initial assessment was unremarkable, and the patient was discharged home with a diagnosis of a viral syndrome. The patient continued to have headaches and fevers; 1 week later, the patient was found at home by her mother unresponsive and uncommunicable, and the patient's mother called 911.
Upon arrival, the patient's mother also said the patient had lost 13.6 kg (30 lb) in the past 3 months. The patient was born in the Philippines, moved to the US at the age of 3, and the last time the patient was in the Philippines was 2 years ago. Five months before the visit, the patient had a positive PDD - purified protein derivative test (also known as the Mantoux test) and had been taking isoniazid for a 9-month course.
Neurological examination, the patient is in a state of drowsiness, eyes open naturally but not as requested. Cranial neurologic examination was difficult because the patient was somnolent, but the patient had limited lateral vision. The patient had a correct localized response to painful stimuli in all extremities, and the patient had a right-sided Babinski sign.
The remarkable test for serum sodium is 124 mEq/L. First cranial CT without contrast showed hydrocephalus with transmeningeal flow. CSF has 227 WBCs/mm3 (60% lymphocytes), protein is 140 mg/dL, and glucose is 29 mg/dL. CT of the chest, abdomen, and pelvis were unremarkable. Brain MRI showed increased meningeal enhancement (including the meninges at the base of the skull) and hydrocephalus.
The patient underwent surgical placement of ventricular–peritoneal drainage, and although microscopy and cultures of acid-fast bacilli in CSF as well as PCR of Mycobacterium tuberculosis were negative, the patient was still started on treatment for a single condition. Meningitis was monitored for tuberculosis with isoniazid, pyrazinamide, rifampin, ethambutol, and dexamethasone. The patient completed 12 months of treatment, and, 15 months after the initial visit, the patient gained 22.7 kg (50 lb), participates fully socially, has a part-time job, and there are no cognitive or physical deficiencies.
This case demonstrates how tuberculous meningitis can present with a subacute onset of symptoms and the benefits of initiating antituberculous therapy even when CSF testing is inconclusive. The patient's clinical presentation with recent weight loss, diffuse meningitis on MRI, hyponatremia, and a recent positive PDD test raises suspicion for tuberculous meningitis.
4.Conclusion

TB in general and tuberculous meningitis are found mostly in countries with high rates of poverty, malnutrition, and low income and can be difficult to diagnose. Diagnosis is most effectively made through a combination of testing for CSF using traditional diagnostic methods, such as Ziehl-Neelsen staining (acid-fast bacilli) and culture of mycobacteria, and by new technologies. Because TB diagnosis is often delayed by several weeks, empiric treatment should be initiated when CNS TB is suspected.
When possible, TB infection should be confirmed by CSF or other tissue culture and drug susceptibility should be determined, as antituberculosis treatment should be adjusted if MDR-TB or MDR-TB is detected. Concomitant steroid therapy should be indicated for all patients with tuberculous meningitis and should be strongly considered in other forms of CNS tuberculosis with edema.
Although HIV coinfection usually does not alter the neurologic or radiologic manifestations of CNS TB, ART may influence the natural course of CNS TB (eg. , IRIS), therefore HIV infection status should be determined in all TB-infected patients.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, a system of modern equipment and technology. The hospital provides comprehensive and professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.