This is an automatically translated article.
The article is professionally consulted by Master, Doctor Tong Van Hoan - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital.Ventilator-associated pneumonia is one of the most common clinical problems in the intensive care unit, reducing the patient's prognosis as well as increasing the cost of treatment. Therefore, treatment of ventilator-associated pneumonia requires active prevention and, when faced with patients with ventilator-associated pneumonia, it is important to optimize antibiotic therapy and comprehensive care.
1. How to initiate and choose antibiotics?
Antibiotics are central to the treatment of ventilator-associated pneumonia. Even in patients with a protracted prognosis, antibiotics are often initiated early. Some evidence is well documented that delayed antibiotic treatment may increase the incidence of ventilator-associated pneumonia as well as mortality in patients with the disease.
The antibiotic to be selected initially needs to be able to fight the epidemiological universal pathogens in the health care facility. In addition, antibiotic choice should also be based on the patient's prior antibiotic exposure, the patient's comorbidities, and the length of hospital stay. In this regard, special consideration should be given to patients with concurrent medical care-associated pneumonia, as pathogenic strains have a high probability of being multidrug-resistant pathogens. Risk factors for acquiring multidrug-resistant pathogens to investigate when initiating antibiotic selection include: recent hospitalization within 90 days, residency in a nursing home or long-term care facility recent history of intravenous antibiotic therapy, chemotherapy or wound care within the last 30 days of current infection, or the patient on hemodialysis.

Antibiotic regimens in patients with ventilator-associated pneumonia are broad-spectrum antibiotics, always with a multi-group combination to increase bacterial control on multiple mechanisms; Sometimes antifungal agents are also needed. It should be emphasized that the initial use of narrow-spectrum antibiotics should not be used because it will increase antibiotic resistance and make it difficult to choose the next antibiotic when resistance is present.
2. How to predict disease-causing organism?
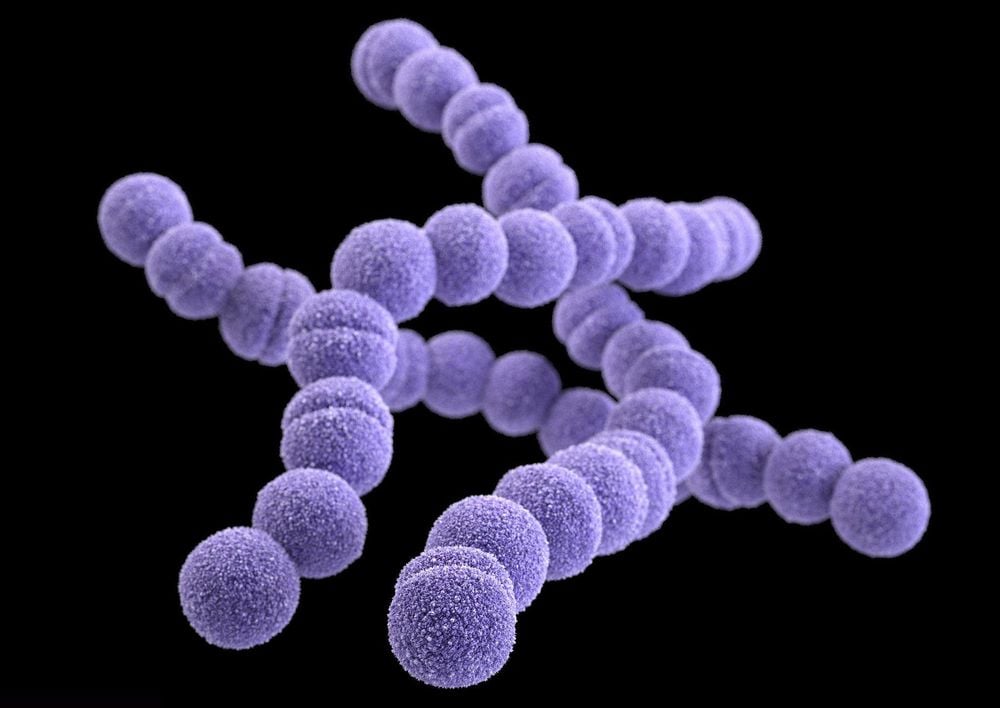
In general, the main pathogens of ventilator-associated pneumonia in healthcare settings are Pseudomonas aeruginosa and Staphylococcus aureus. However, if the patient has early onset of ventilator-associated pneumonia, which is within the first 4 days of invasive respiratory intervention, the bacterial strain may also be the common causative agent of community-acquired pneumonia. such as S. pneumoniae, S. aureus and H. influenzae. In contrast, the causative agent of late ventilator-associated pneumonia was largely aerobic Gram-negative bacilli, mainly P. aeruginosa, Acinetobacter baumannii or methicillin-resistant S. aureus. In addition, microbiological differences were seen in postoperative or neurosurgery patients, in which S. aureus was frequently reported as the main pathogen.
In addition, a multicenter study showed that the prevalence of resistant microorganisms in patients with ventilator-associated pneumonia is high. Therefore, antibiotic initiation strategies should be based on accurate guidelines for local epidemiology in order to predict the causative organism. At the same time, the suction of endotracheal fluid for bacterial culture should also be encouraged from the time of intubation in order to accurately orient the causative agent and facilitate the next step of antibiotic selection.
3. How long is antibiotic treatment?
Standard duration of antibiotic therapy has been shown to be effective in critically ill patients with ventilator-associated pneumonia with progression to severe sepsis, particularly when dialysis interventions are required. or extracorporeal circulation. Accordingly, the duration of antibiotic treatment in ventilator-associated pneumonia is at least 7 days, usually 14 days and sometimes up to 21 days.
Conversely, if the duration of antibiotic therapy is inadequate, although clinical symptoms may improve, the persistence of bacteria that has not been completely resolved increases the risk of developing pneumonia and developing pneumonia. antibiotic resistance.
A novel approach to antibiotic treatment for ventilator-associated pneumonia is nebulization of antibiotics in addition to the usual systemic administration. The advantage of this pathway is that it allows high topical antibiotic concentrations to be achieved, with rapid clearance, with reduced risk of resistance, and with minimal absorption resulting in less toxicity. Therefore, patients will shorten the time of taking the drug, reduce the possibility of re-infection. Antibiotics that can be used by nebulization are colistin, polymycin or aminoglycosides. However, this route of administration is never monotherapy; At the same time, to ensure effectiveness, the artificial respiratory system as well as the breathing mode must be appropriate, helping to disperse the drug into the patient's alveoli.
4. Other comprehensive treatments for ventilator-associated pneumonia
4.1 Nutrition, respiratory capacity and position Enteral feeding is now being encouraged as early as possible in postoperative patients. The reason is that this is the natural digestive tract, ensuring the patient is fully absorbed nutrition and preventing ventilator-associated pneumonia compared with prolonged intravenous feeding.

The patient's breathing capacity and posture have also been shown to have a relationship with the risk of ventilator-associated pneumonia. Accordingly, placing the patient in a lying position with the upper half of the body higher will reduce the risk of hospital-acquired pneumonia by about 3 times, especially when feeding enteral. In addition, the frequent rotation and active back patting also contributes to the elimination of viscous sputum and avoids stagnation of inflammatory fluid.
4.2 Prevention of stress-induced gastrointestinal bleeding gastrointestinal bleeding. Therefore, the protection of gastric mucosa with proton pump inhibitors, H2 receptor blockers and sucralfate has shown remarkable results, especially in cases of ventilator-associated pneumonia. late.
4.3 Prevention of DVT In patients requiring prolonged mechanical ventilation, DVT prevention is indicated and the choice of method should be based on individual patient characteristics and pathology. go with. Commonly used agents, low-molecular-weight heparin, new-generation anticoagulants, and compression stockings are proven effective means of helping to prevent deep vein thrombosis of the lower extremities in patients.
In summary, treatment of ventilator-associated pneumonia should be aggressive from the outset with antibiotic therapy appropriate to the causative agent, the patient's risk factors, and comprehensive supportive care. . The antibiotic duration should be long enough to ensure the ability to control bacteria and closely monitor the ability to improve on clinical and biochemical signs to take timely corrective measures for the patient.
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














