This is an automatically translated article.
Article written by MSc Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International Hospital
For the treatment of tuberculous meningitis, WHO recommends a combination of drugs and drug duration similar to those of pulmonary tuberculosis: 2 months of rifampin, isoniazid, pyrazinamide, and ethambutol, followed by 10 months of rifampin and isoniazid.
1.Treatment Empiric therapy should be initiated if CNS TB is suspected rather than waiting for a definitive diagnosis, with treatment based on HIV infection status and affected organ susceptibility. TB.
Unfortunately, determining this susceptibility requires a nucleic acid test that can detect M. tuberculosis along with the gene mutations associated with drug resistance, such as the rpoB gene mutations associated with rifampin resistance , or traditional bacterial cultures (cultures are usually not valid if treatment has been in place for several weeks or months). Of the available antituberculous drugs, isoniazid and pyrazinamide have the best penetration into the subarachnoid space:
Isoniazid : a CSF/serum concentration ratio of 40% with normal meninges, and CSF concentrations similar equivalent to serum concentrations during meningitis. The dose is 10 mg/kg/day orally for adults (administered together with oral pyridoxine 50 mg/day to 100 mg/day). Rifampin: the CSF/serum ratio is poor when meninges are normal and 20% when meninges are inflamed (lower than the minimum inhibitory concentration for M. tuberculosis that is susceptible to the whole drug). The dose is 15 mg/kg/day orally for adults. Ethambutol: The CSF/serum ratio is poor if the meninges are not inflamed, but appropriate minimal inhibitory concentrations can be reached in the presence of meningitis. The usual dose is 15 mg/kg/day orally; Higher doses of 25 mg/kg/day to 35 mg/kg/day achieved better minimal inhibitory concentrations but increased the incidence of optic neuritis (2% at 25 mg/kg/day by mouth). ). Pyrazinamide: CSF/serum ratio similar to isoniazid at doses of 30 mg/kg/day to 35 mg/kg/day orally. Streptomycin: CSF/serum ratio is close to zero if the meninges are not inflamed and poor even in the presence of meningitis. The dose is 1 g/day IM in adults.

2. Drug-resistant TB Treatment of all forms of TB has been complicated by the emergence of drug-resistant TB. Multidrug-resistant TB is defined as tuberculosis resistant to isoniazid and rifampin. Although MDR-TB can be transmitted to others, it is most common in a patient with fully susceptible TB who has not completed treatment.
Super drug-resistant TB is defined as TB resistant to isoniazid, rifampin, and one antibiotic in the quinolone family, and at least one of the second-line drugs kanamycin, capreomycin, or amikacin.
Both multidrug-resistant and super-resistant TB have been detected in all regions of the world. WHO recommends that all patients with MDR-TB or MDR-TB receive a directly monitored treatment strategy plus a second-line anti-TB drug.
3. Treatment in HIV-coinfected patients For patients newly diagnosed with TB and HIV, if CD4+ T-cell counts are less than 50 cells/mm3, early initiation of antiretroviral therapy (ART) ) will reduce mortality and the risk of opportunistic infections; For patients with a CD4+ T-cell count of 50 cells/mm3 or higher, HAART should be started 2 to 12 weeks after starting TB treatment.
Some anti-tuberculosis drugs, such as rifamycins, may decrease serum concentrations of protease inhibitors and some non-nucleoside reverse transcriptase inhibitors, potentially inactivating these substances.
In 2017, WHO reaffirmed its recommendations for HIV therapy in patients coinfected with TB: (1) HIV treatment should be initiated regardless of the CD4+ T-cell count; (2) TB treatment should be initiated first, followed by ART as soon as possible within the first 8 weeks of treatment; and (3) severely immunocompromised patients (eg, CD4+ T-cell counts less than 50 cells/mm3) requiring ART within the first 2 weeks of TB treatment.
4. Paradoxical expansion Paradoxical expansion is defined as an increase in the size of an existing TB tumor or the appearance of a new TB tumor despite appropriate anti-TB treatment; This extension usually occurs within 3 months of starting treatment and is accompanied by neurologic deterioration. Paradoxical spread in HIV-infected and HAART-treated patients suggests that immune remodeling may contribute to paradoxical spread.
In a report of 23 patients with paradoxical spread, one patient died, approximately 25% had residual neurological symptoms, and less than one third required surgical intervention. Although there are no randomized trials of corticosteroid therapy for paradoxical spread, most experts believe that corticosteroids improve neurological symptoms and treatment outcomes, and argue that anti-TB therapy should be prolonged. up to 12 to 18 months.

5. Corticosteroids The use of corticosteroids has gained increasing acceptance and is recommended as a concurrent treatment for CNS TB (Clinical case presented below), especially for patients with peritonitis. TB brain.
A meta-analysis of 07 randomized controlled trials comparing antituberculosis treatment with or without corticosteroids concluded that “Corticosteroids reduce mortality from TB meningitis, at least in the short term”.
In the 2017 “Guidelines for the Treatment of Drug-sensitive TB and Patient Care,” WHO recommends initiating adjuvant corticosteroid therapy with dexamethasone or prednisolone tapered over 6 to 8 weeks for all patients with meningitis due to TB.
In animal models, corticosteroids reduce intracranial pressure and reduce inflammation in the subarachnoid space, cerebral hemispheres, spinal cord, and small blood vessels. The theoretical adverse effect of corticosteroids stems from a reduction in meningitis, which in turn is likely to decrease the permeability of anti-tuberculosis drugs; then from suppressing the immune system, which can lead to bacterial superinfection; or from worsening TB or other complications related to corticosteroid use, such as gastrointestinal bleeding.
Recent research suggests that polymorphisms in the leukotriene A4 hydrolase (LTA4H) gene, which encodes a protein that affects the production of leukotriene B4 (an inflammatory eicosanoid), impacts inflammation risk in patients with meningitis tuberculosis; The rs17525495CT polymorphism determines inflammation, with patients with homozygous TT genotype having the strongest degree of inflammation.
If corticosteroids are indicated, dexamethasone is most commonly used at doses of 12 mg/day to 16 mg/day for 3 weeks, then tapered over 3 weeks. For patients who worsen while on dose reduction, corticosteroids may be used for a longer period of time. Repeated neuroimaging in patients with tuberculous meningitis demonstrated that dexamethasone-treated patients had fewer complications with hydrocephalus and cerebral infarction.
Case
A 44-year-old male patient presents with a 2-week history of back pain, headache, confusion, and intermittent loss of consciousness. The patient moved to the US from China 7 years ago. Notable family history with one brother who died of central nervous system tuberculosis. Neurological examination showed mild reflex asymmetry in the biceps muscles.
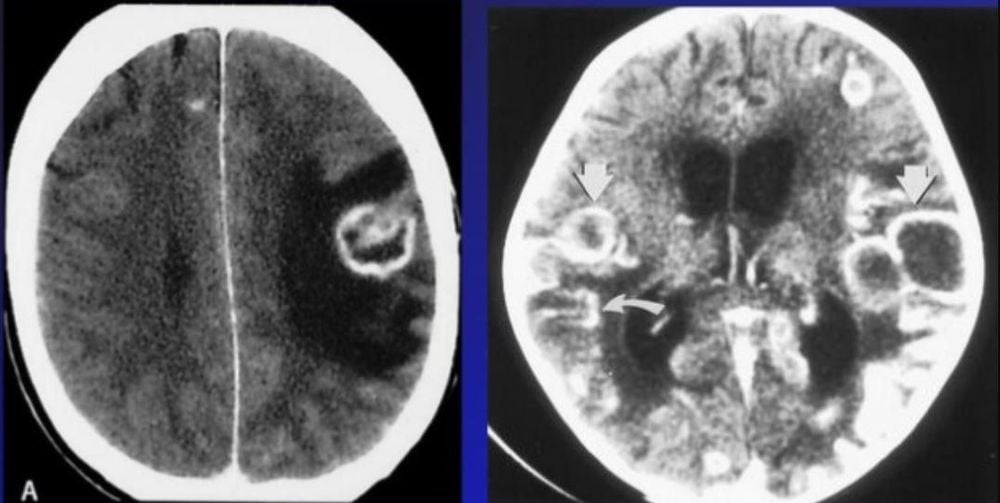
MRI of the spine showed osteomyelitis in vertebra L4 with right paravertebral abscess and osteomyelitis in T9-T10 vertebrae. Brain MRI showed multiple ring-shaped enhancement lesions, all less than 1 cm in diameter, in the brainstem, brainstem, and cerebellum.
In addition, the large lesions seen in the left pons and medial thalamus extend into the third ventricle. The patient was biopsied for osteomyelitis in the spine, the results were positive for acid-fast bacilli; cultures of acid-fast bacilli in CSF were positive for fully susceptible Mycobacterium tuberculosis. Chest and abdominal radiographs showed no significant abnormalities.
The patient was initiated on isoniazid, rifampin, pyrazinamide, and ethambutol, with adjuvant dexamethasone, and seizure prophylaxis phenytoin, and, at first, the patient improved markedly.

Subsequent MRI with gadolinium injection showed a reduction in the size of the ring-enhanced granulomas. The patient subsequently developed elevated liver enzymes and treatment was switched to capreomycin, moxifloxacin, ethambutol, cycloserine, and dexamethasone. The patient then developed tinnitus, and capreomycin was continued.
The following week, the patient developed oral candidiasis and agranulocytosis, and the dexamethasone dose was gradually reduced and the phenytoin dose kept unchanged.
One week later, the patient experiences increased somnolence, headache, and vomiting; dexamethasone dose was increased again and symptoms improved. After 12 months of treatment, MRI with gadolinium injection showed all ring-shaped enhanced granulomas.
Patient has no symptoms and returns to work. Speech in Chinese is fluent, and the patient has no motor impairment or reflex asymmetry, and when walking there are times when the feet are in a straight line.
Comment:
This case demonstrates a prolonged delay between the time of arrival in the US from a country where TB is endemic (China) and the onset of CNS TB in the US.
In addition, although the treatment of this patient was challenging because of the many complications due to drug toxicity, the clinical course remained very good with almost complete recovery, demonstrating that despite the numerous granulomatous TB, the long-term outcome of CNS TB can still be quite good. Close follow-up in a TB clinic is necessary to recognize the common side effects of TB treatment.
6. Treatment Outcomes In the era of streptomycin and isoniazid, 32% of children with tuberculous meningitis died and 24% of survivors had neurological sequelae, including hemiplegia, quadriplegia and spastic paralysis. limb, ataxia, or cognitive impairment; 58% had hearing loss, but all were treated with streptomycin, an ototoxic aminoglycoside.
Currently, the results of treatment for tuberculous meningitis are correlated with the neurological status at the time of medical examination. The British Medical Research Council has defined three stages of tuberculous meningitis.
Stage 1 includes patients who are conscious and have no neurological deficits or hydrocephalus; Meningeal irritation may occur. Stage 2 includes patients with confusional consciousness and focal neurological deficits. Stage 3 includes patients with stupor or coma and hemiplegia or paraplegia.
All stage 1 patients at the time of diagnosis will survive with some neurological sequelae, while nearly 25% of stage 2 or stage 3 patients die or have severe neurological sequelae .
Intracranial vascular disease is common in tuberculous meningitis, and stroke can occur as a complication of vasospasm, thrombosis, vasculitis, or hemorrhagic infarction. The arteries most commonly affected are the middle cerebral arteries and their branches. The outcome of TB treatment with appropriate anti-TB therapy is good, with a mortality rate of less than 10%.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles refer to the source:
Zunt JR. Tuberculosis of the Central Nervous System. Continuum (Minneap Minn) 2018;24(5, Neuroinfectious Disease):1422–1438.