This is an automatically translated article.
The article was consulted with Specialist Doctor I Dang Thi Ngoc Chuong - Department of Pediatrics - Neonatology, Vinmec Central Park International General Hospital.Neonatal respiratory failure is a respiratory dysfunction that results in hypoxia and increased CO2 in the blood. It is the leading cause of infant death. Treatment of neonatal respiratory failure must be done quickly to prevent respiratory failure, acidosis, infection, exhaustion, along with treatment of the cause.
1. What is neonatal respiratory failure?
Respiratory failure is a dysfunction of the respiratory system due to many causes. This can lead to hypoxia and increased CO2 in the blood, thus no longer able to maintain PaO2, PaCO2, pH at acceptable levels, consequent failure of gas exchange.Neonatal respiratory failure is the most common syndrome and the leading cause of neonatal mortality, requiring prompt emergency care and proper management.
2. Causes of acute respiratory failure in infants
Causes of neonatal respiratory failure can originate from respiratory causes, can also be caused by extra-respiratory causes:Causes in the respiratory tract:
Common: endothelial disease, aspiration syndrome, Intrauterine pneumonia, delayed pulmonary drainage, pulmonary hypertension. Uncommon: pulmonary bleeding, pneumothorax, pulmonary hypoplasia. Rare: Congenital air cocoon, posterior nostril occlusion. Causes outside the respiratory tract:
Defects: thoracic malformation, congenital heart, diaphragmatic hernia. Metabolic disorders: hypoglycemia, hypothermia, acidosis. Nervous system diseases: intracranial hemorrhage, meningitis, morphine poisoning... Due to circulation: acute blood loss, polycythemia vera.

3. Treatment of neonatal respiratory failure
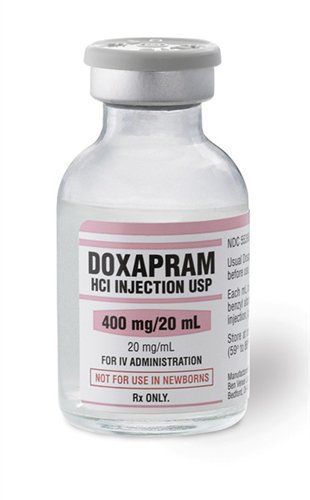
Treatment of neonatal respiratory failure should be carried out immediately based on the following principles:Anti-respiratory failure Anti-acidemia Anti-infective Anti-exhaustion Treat cause. 3.1. Preventing respiratory failure The doctor can take one or more measures to prevent respiratory failure and provide oxygen to the child such as:
Aspiration of the nose and throat. Put the child in the airway position: head slightly tilted back, can put a thin pillow under the shoulder. Stimulate baby to breathe Keep warm Drain the stomach to help reduce bloating. Provide oxygen immediately: depending on the degree of respiratory failure, choose different methods: breathing oxygen through a tube, through a mask, endotracheal tube or giving the child a ventilator to support. Monitor the child's transdermal oxygen saturation (92 - 95%) to adjust the inhaled oxygen concentration. Extracorporeal membrane oxygenation (ECMO) technique for the treatment of neonates with severe respiratory failure:
Methods to help support life function in patients with circulatory or severe respiratory failure, poor response or even unresponsive to conventional resuscitation measures. Place a vascular cannula (catheter) and connect it to an ECMO machine system to deliver oxygen across the extracorporeal membrane, thereby transferring oxygenated blood into the body's circulatory system to supply oxygen to tissues and organs in the body. young body. When the child's respiratory failure improves, the patient can be extubated if breathing is good on oxygen support. Use of Nitric Oxide gas in the treatment of severe respiratory failure in infants
Good use in severe respiratory failure due to causes such as: Meconium aspiration pneumonia, endocardial disease, primary pulmonary hypertension, sepsis ,.. NO breathing technique has shown good effectiveness in improving blood oxygenation, saving the lives of children with life-threatening severe respiratory failure, with almost no side effects. Patients with high pH and low oxygen index (OI) have a better response to NO inhalation than conventional supportive methods. 3.2. Anti-acidosis Alkaline compensation based on blood gas results is ideal when the infant is well ventilated.
Number of mEq (Sodium bicarbonate) = BE x P x 0.3 (P child weight in kg) In case of respiratory acidosis (PaCO2 > 70 mmHg), the patient can be discharged with CO2 by ventilator When blood gas is not available then can be compensated by the formula 2mEq/kg. Hct > 65% (venous blood) → partial exchange 3.3. Prevention of infection Ensuring hygiene in child care is extremely important, especially in cases of intubation. Physicians may consider giving patients broad-spectrum antibiotics when respiratory distress is associated with premature rupture of membranes, foul-smelling amniotic fluid, maternal fever before delivery, or when it is difficult to differentiate between pneumonia and other causes. It is best to use antibiotics according to the antibiogram.
3.4. Anti-burnout Prevention of burnout for children needs to pay attention to the basic issues:
Ensure the child's body temperature is at 36.5 - 37 degrees Celsius. Provide warm and humid oxygen. Provide enough energy for children. Anti-low blood sugar.
Delayed digestion of pulmonary fluid Common in babies born by cesarean section without labor, babies born too quickly or mothers who use β-blockers. The X-ray picture of the lungs is not bright because the alveoli still contain a lot of fluid, you can see less fluid at the pleural angle, thickening the interlobular groove.
Usually the respiratory failure improves within 24 hours of treatment. If after 24 hours the child is still dependent on oxygen, these are cases of increased surfactant consumption or inadequate excretion of surfactant. At that time, the patient can be given continuous positive airway pressure and consider using surfactant.
Meconium aspiration syndrome This condition is common in fetuses past due date. Meconium spills into the respiratory tract, obstructing ventilation, blocking the airway. In addition, the air from inside the lungs can accumulate in the chest cavity and around the lungs causing pneumothorax, making it difficult to regenerate the lungs... meconium amniotic fluid. Children have symptoms of respiratory failure: rapid breathing, difficulty breathing, whining, cyanosis, apnea, slow heart rate, decreased muscle tone. On the X-ray film, there are alternating areas of the lung with opacity and the area of increased light, possibly with a collapsed lung area.
At this point, the child must be immediately aspirated through the bronchoscope until the meconium fluid can no longer be aspirated. Intubate a surfactant pump as soon as possible. Use broad-spectrum antibiotics and prevent complications of pneumothorax.
Intrauterine pneumonia Common in infants infected by antenatal streptococcal B, E.Coli. Chest X-ray showed bronchopneumonia. Treatment in this case requires broad-spectrum antibiotics, respiratory support, and a surfactant pump may be considered.
Pulmonary bleeding is a secondary disease after prolonged severe hypoxia or coagulopathy. Children have respiratory failure, pink foam, fresh blood spurts through the nose and mouth and die very quickly.
Management: Intubation, ventilation with PEEP 7-8 cmH2O, fresh blood transfusion, anti-coagulation disorder, surfactant can be used.
Inner membrane disease A functional deficiency of surfactant in the lungs, common in very premature infants. Respiratory failure appears soon after birth, the baby has rapid, shallow breathing, shrinks and cyanosis very quickly if not treated promptly
Treatment: respiratory support with CPAP machine or ventilator, Use surfactant 100-200 mg/kg/dose. Repeat dose after 6-12 hours if the child still has signs of severe respiratory distress and does not reduce the need for FiO2, or the chest X-ray is still fuzzy and the lung compliance is poor.
Respiratory distress syndrome in premature infants is often treated with the technique of supplementing with surfactant compounds. As before, medicine often uses the technique of endotracheal intubation with Surfactant and mechanical ventilation for children. Today, the Surfactant pump technique for treating neonatal respiratory failure is less invasive and increasingly widely used. Currently, there are many different methods and techniques of surfactant injection, which should be considered on a case-by-case basis.
Surfactant pump technique to treat respiratory failure in newborns has been implemented at Vinmec International General Hospital. The benefits of this therapy are: improved lung ventilation, increased blood oxygenation, reduced frequency of air leaks (complications with pneumothorax, alveolar congestion...), reduced mortality and morbidity. for kids...
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.