This is an automatically translated article.
The article is expertly consulted by Master, Resident Doctor Dang Thi Ngoan - Pediatrician - Neonatologist - Department of Pediatrics - Neonatology - Vinmec Ha Long International Hospital.Acute intussusception in children is a common surgical emergency, which can cause many dangerous complications and even death if not treated promptly. Children with intussusception can be at any age, but are most common in children under 2 years of age, and are most common in children between 4 and 9 months of age.
1. Overview of acute intussusception in children
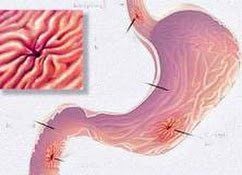
Acute intussusception in a child is a common surgical emergency, occurring when a segment of the child's intestine turns and enters the lumen of the adjacent bowel, causing mechanical obstruction. There are many types of intussusception, but the most common is the ileocecal intussusception.
Children with intussusception can be at any age but are most common in children under 2 years of age, most often in those between 4 and 9 months. The disease is common in chubby and fat children, less common in malnourished children. The rate of intussusception is 2 to 4 times more common in boys than in girls. The frequency of acute intussusception in Vietnamese children is 3 cases per 1000 children under one year of age/year.
Children with intussusception often have no known cause. Possibly due to an imbalance between the size of the ileum compared with the ileocecal valve, due to lymphadenitis of the mesentery, some cases of acute intussusception started with Meckel's diverticulum, polyps, small bowel tumors, and tumours. worms,...
In terms of prognosis, the progression of intussusception is very different in the two age groups. In particular, for nursing infants with intussusception (under 24 months old), the disease will progress rapidly, acutely, and become severe hour by hour. In older children, the manifestation of subacute or chronic disease is not as severe as in nursing infants.

Manifestations of intussusception parents should pay attention to are:
Abdominal pain: When abdominal pain appears, the child cries suddenly, violently, twisting, the pain makes the child stop playing, stop feeding. Vomiting: appears from the first pain, at first the child vomits food, then may vomit green or yellow fluid. Blood in the stool: can appear soon after the pain or appear late after 24 hours. Breastfeeding infants with intussusception 95% have symptoms of bloody stools. If taken to hospital late, the child may have bowel necrosis, intestinal perforation causing peritonitis, infection, and toxicity. At this time, the child will have pale skin, fatigue, high fever, little urine, lethargy, coma.
2. Treatment of intussusception in infants and young children
2.1. Principles of treatment of intussusception in children
The principle of intussusception treatment is to resuscitate the child, remove the intussusception as soon as possible and treat the cause of the intussusception if any.
Regarding medical resuscitation, the child will be placed with a nasogastric tube to drain, fasting. Add water and electrolytes if there is a disorder. Use antibiotics Ceftriaxon or Cefotaxime, can be combined with Metronidazol.
Regarding intubation, there are two methods: air intubation and surgical removal.

2.2. Methods of intussusception to treat intussusception in infants and young children
2.2.1. Steam cage removal method
Inflatable is an effective method of intubation when the child has not had complications such as intestinal perforation, bowel necrosis, intestinal obstruction,... The child is placed through a nasogastric tube and rectal catheter, then anesthetized. Air is mechanically injected into the rectal catheter to expel the intussusception, which is performed under the observation of an X-ray monitor. Standard inflatable pressure is 60-120 mmHg (start with 60-8 mmHg and then increase gradually). Each inflation should not last more than 3 minutes and do not remove more than 3 times. This is a simple trick but the success rate is high (over 90%). Signs of successful intubation are: the abdomen is round and round, the intussusception is not palpable, the pressure column on the machine drops suddenly, the symptoms of bowel obstruction improve. After successfully removing the cage, the baby can eat and drink again after 2 hours. The child will be kept in the hospital for a few hours to monitor symptoms such as abdominal pain, vomiting, fever, defecation, ... to detect recurrent intussusception or complications after removal of the intussusception. Children are usually discharged the same day.

2.2.2. Surgical method to remove the cage
Surgical intussusception is indicated when air intubation has failed or the child has had complications. Surgery also helps to deal with the physical causes of acute intussusception such as Meckel's diverticulum, polyps, small bowel tumors,...
There are two surgical methods: laparoscopic surgery and open surgery. Depending on the case, the doctor will choose the right method for the child. Laparoscopic surgery is indicated in cases of acute intussusception in children with failed intussusception without complications or in chronic intussusception with a physical cause.
For open surgery, there are two approaches:
If the location of the intussusception is in the right colon, the doctor will make a transverse incision above the right navel. If the location of the intussusception is in the left colon or is unknown, the doctor will perform surgery in the midline white line. Regarding the treatment of the intussusception during surgery, if the intussusception has not been necrotic, the doctor will remove the cage. Depending on the condition of the damaged intestine, the doctor will cut the intestine or just cover it with warmth, and find and treat the cause of the child's intussusception. If the intussusception is already necrotic, perform an intestinal anastomosis to remove the entire intussusception.
Depending on the surgical intervention, the child may have to temporarily fast for 24-48 hours. Your child will continue to receive rehydration, electrolytes, pain relievers, and antibiotics. The nasogastric tube is withdrawn at the onset of bowel movements, and the child is considered for re-feeding. Children are usually discharged after 3-7 days.
3. Common complications after intussusception and prognosis
Complications that can be encountered during intubation treatment are enteritis, intestinal perforation,... Post-operative complications are enteritis, anastomosis, bowel necrosis, septic shock, and water disturbances. electrolytes,...
Regarding the prognosis, the rate of recurrence of acute intussusception in children after air intubation is 10-15%, recurrence may appear after a few hours or after several years. After surgical treatment, there is also a risk of recurrence, but the rate is lower.
Currently, the cause of intussusception in children has not been found, so there is no specific preventive measure. The best way is for parents to recognize abnormal signs in their children to detect intussusception early and avoid dangerous complications caused by the disease. Accordingly, when seeing a child showing signs of intermittent abdominal pain, manifested by sudden, intense crying, hunching over, refusing to suckle, twisting, stopping playing, etc., parents need to immediately take them to the hospital. children go to the doctor. Doctors will examine and diagnose the child to confirm the diagnosis and take timely intervention measures for the child.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
| Đăng ký tư vấn dinh dưỡng cho bé tại: https://i.vinmec.com/dangkytuvandinhduong |
|---|














