This is an automatically translated article.
Acute malnutrition in children is increasing. The disease needs to be detected in time for early and effective treatment, otherwise it will lead to life-threatening.
1. What is acute malnutrition?
Acute malnutrition is a medical condition in which the body does not receive enough energy and protein according to the needs due to lack of supply or disease, causing children to lose weight rapidly, stunted or edematous.
If children have acute malnutrition, the risk of death is 5 - 20 times higher than that of normal children and can be a direct cause of death in children or can play an indirect role in increasing rapidly risk of death in children with common illnesses such as diarrhea and pneumonia .
2. Treatment of acute malnutrition in children
To treat acute malnutrition, it is necessary to consider the extent, there are 3 levels of malnutrition: mild malnutrition, moderate malnutrition, severe malnutrition.
Treatment of acute malnutrition has 3 types: inpatient treatment, outpatient treatment, maintenance treatment. In addition, treatment depends on the occurrence of complications as well as the degree of acute malnutrition.

Tùy thuộc vào tình trạng của trẻ để có phương án điều trị phù hợp
2.1. Inpatient treatment Acute malnutrition in children with complications, severe disease that does not respond to outpatient treatment will be treated as inpatient in hospital. Inpatient treatment is divided into two phases:
Emergency stage for children when they fall into an acute condition and are seriously injured. In this case, the child will have hypoglycemia, hypothermia, electrolyte disturbances, infections, micronutrient deficiencies. When entering the emergency room, the child will be treated by the doctor with the following steps:
Step 1: Treat hypoglycemia with special caution when using intravenous lines for children. Step 2: Treat hypothermia to ensure that the child is warm enough, using therapeutic nutritional products. Step 3: Treat dehydration using preparations, limit rehydration by intravenous infusion. Step 4: Adjust electrolyte balance using rehydration products with low Na content, food should be eaten lightly. Step 5: Treatment of bacterial infections acute malnourished children often have febrile infections, when infected children use antibiotics Step 6: Correct the deficiency of micronutrients, supplement nutrients such as iron, vitamins A, C. The transition period for children with acute malnutrition is the period before transferring the patient to outpatient treatment, in order to effectively manage the child's transition to the recovery stage and give the child the preparation. therapeutic nutrition.

Bổ sung các vitamin và chất dinh dưỡng cần thiết cho trẻ
2.2. Outpatient treatment Outpatient treatment when children have severe acute malnutrition but no complications, treatment is carried out at the primary health care level. Children are given medicines, including antibiotics and RUTF preparations.
2.3. Maintenance treatment Acute malnutrition in children with mild condition without complications. Children are provided with energy and nutrients that may be lacking in meals. In this treatment, children will be vaccinated and dewormed. In addition, children are checked for weight, height, and health care advice.

Cho trẻ uống thuốc tẩy giun định kỳ
3. Measures to prevent acute malnutrition in children
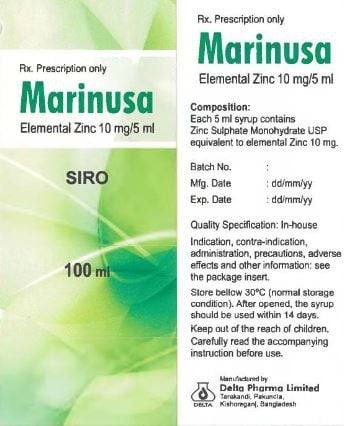
Strengthen communication education to improve nutritional care for mothers and children. Nutrition counseling and care for pregnant women and lactating mothers. Counseling and practice for children to eat complementary foods as recommended. Guidelines for nutritional care for children with stunted growth. Fully vaccinated according to schedule. Iron and vitamin supplements to prevent anemia for pregnant women and children. In addition, to prevent and improve malnutrition in children, parents should supplement with supportive products containing lysine, essential micro-minerals and vitamins such as zinc, chromium, selenium, and B vitamins. meet the nutritional needs of children. At the same time, these essential vitamins also support digestion, enhance nutrient absorption, help improve anorexia, and help children eat well. Parents can also apply dietary supplements and functional foods derived from nature for easy absorption by the baby. The most important thing is that the improvement of the baby's symptoms must take place over the long term. Combining many types of functional foods at the same time or changing many types in a short time can make the baby's digestive system unable to adapt and completely not good. Therefore, parents must be really persistent with their children and regularly visit the website vimec.com to update useful baby care information.