This is an automatically translated article.
Fluid resuscitation is an especially important method of emergency resuscitation, especially for patients with severe sepsis or septic shock. Guidelines for fluid resuscitation vary from country to country, but the most important thing is to ensure the patient's hemodynamics.1. What is the response to fluid replacement?
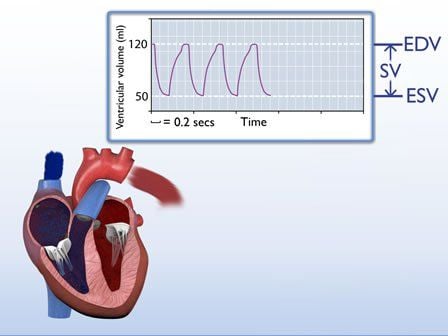
This is the basic principle when deciding to use fluid resuscitation in patients in shock, with hypoperfusion of tissues, and cardiac output. Fluid replacement if increased systolic volume, leading to increased cardiac output, is beneficial.An increase in systolic volume leads to an increase in end-diastolic volume and an increase in mean arterial pressure. Thereby increasing preload and volume.
In contrast, fluid resuscitation that does not increase systolic volume can be harmful:
Too much fluid replacement can cause: tissue edema, organ dysfunction, hypoxia. In sepsis patients with a history of heart failure, when rehydrating about 54% have diastolic dysfunction, 23% have systolic dysfunction causing more severe disease. Left ventricular (LV) overload leads to LV dilation, pulmonary hypertension, pulmonary edema, and left ventricular dysfunction. In fact, diastolic dysfunction often leads to more severe consequences than systolic dysfunction.
Thus, the doctor needs to determine whether fluid resuscitation is beneficial or harmful to the patient? From there, choose appropriate resuscitation as well as take measures and prepare to prevent complications. Patients are considered to be fluid responsive if, after rehydration, there is an increase in systolic volume of at least 10% (usually 500cc of crystalloid) as quickly as possible (usually over 10 minutes).
Patients who respond to fluid resuscitation can continue fluid resuscitation. In patients who did not respond to fluid resuscitation, there was a decrease in systolic or diastolic function, even with a decrease in circulating volume.

Hồi sức dịch là phương pháp hồi sức cấp cứu đặc biệt quan trọng, nhất là với các bệnh nhân nhiễm khuẩn huyết nặng hoặc sốc nhiễm khuẩn
2. How is response to fluid resuscitation determined?
Currently, the passive leg lift test PRL is the only method of determining the response to fluid replacement with high accuracy and is widely used. In fact, it is possible to combine PLR with fluid testing to accurately assess response to fluid replacement. Especially when using a monitor to monitor cardiac output. The PLR is likened to a fluid bolus, which causes venous displacement of blood from the lower extremities to the thoracic cavity.2.1 Advantages Non-invasive. Reversible. The amount of fluid varies with body size. Can be used regardless of ventilation mode and heart rate. 2.2 Disadvantages Not effective in patients with high intra-abdominal pressure. May be contraindicated to change position. Other interventions may have to be discontinued during PLR implementation.
3. Some things to know about the response to fluid resuscitation
Determination of response to fluid resuscitation: clinical signs, CVP, chest X-ray, and ultrasonography were judged to be imprecise and not used.Clinical signs
May indicate tissue hypoperfusion but cannot indicate patient response to fluid resuscitation.
CVP Indicators such as CVP or mean arterial pressure (MAP) are also inaccurate in assessing fluid resuscitation response.
Ultrasound Ultrasound is currently being evaluated as a new, potential means of assessing volume status and fluid resuscitation response. With respect to volume status, there are studies on measuring IVC in ventilated patients, but not in spontaneously breathing patients. 2016, Lee presented an evidence-based algorithm to guide the decision to resuscitate on IVC based on the available literature.

Siêu âm hiện được đánh giá là phương tiện mới, có tiềm năng trong đánh giá tình trạng thể tích và đáp ứng hồi sức dịch
In addition, Marik has proposed another method to evaluate fluid resuscitation such as LVOT time analysis ultrasound (VTI), change in pulse pressure measured in the radial pulse, transesophageal Doppler, biological response.
The hemodynamic response to fluid resuscitation is usually short and minimal, and within 30 minutes, the cardiovascular index will usually return to baseline. An increase in MAP after fluid resuscitation is a minimal condition; if an increase in systolic volume and cardiac output is not observed, fluid bolus should not be observed.
Patients should only receive fluid bolus if the hemodynamic benefit outweighs the risk of fluid overload. However, it should be noted not to continuously rehydrate, which can easily cause fluid overload. Instead, use vasopressors, relieve pain early, limit angioedema and increase organ perfusion.
The main factors affecting organ perfusion are CVP and MAP. Current fluid resuscitation guidelines require maintaining the patient's CVP greater than 8mm Hg.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.