This is an automatically translated article.
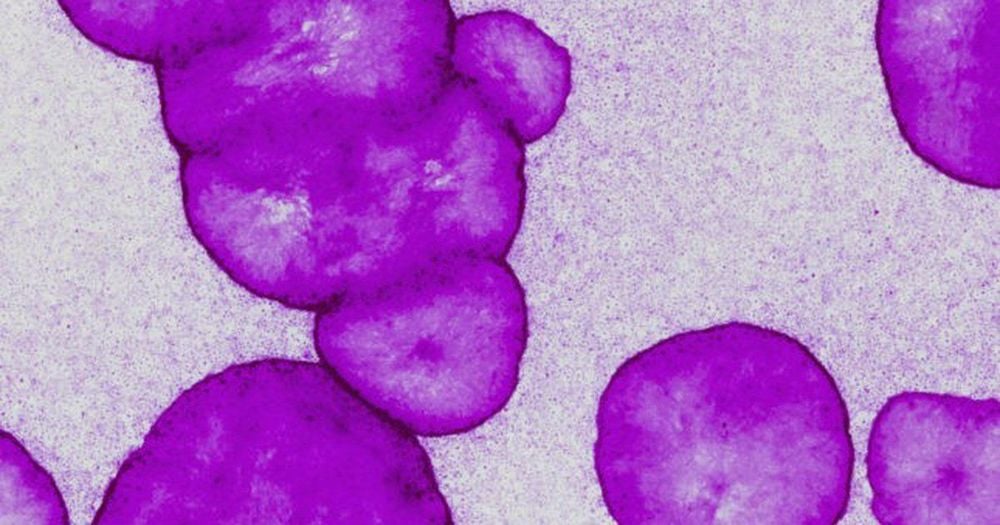
The article was professionally consulted with Specialist Doctor I Tran Van Sang - Dermatologist - Department of Medical Examination & Internal Medicine - Vinmec Danang International General Hospital.Epidermolysis bullosa is the common name for a group of rare, genetic disorders. The common feature of the disease group is the appearance of blisters on the skin or mucous membranes after mild trauma. Different diseases will have different severity and symptoms of epidermolysis bullosa.
1. What is epidermolysis bullosa?
Epidermolysis bullosa is a common name for a group of rare, genetic disorders with an incidence of 19.6/1 million newborns in the United States. The common manifestation of the disease group is the appearance of blisters after mild trauma to the skin and mucous membranes. Different clinical forms of the disease will have different scar healing process. The healing process can be abnormal, forming chronic erosions, scars, overgrown granulomatous tissue, and even invasive cancers. Mild clinical forms may have little or no effect on internal organs. However, severe clinical forms, recessive genetics often greatly affect internal organs, seriously affecting health, reducing the patient's life expectancy.The cause of the disease is a genetic mutation that causes a disorder in the formation of essential components of the basal membrane region. In the structure of the skin, the basement membrane area helps to bond between the epidermis, the top layer of skin, and the dermis. The basement membrane area of people with epidermolysis bullosa is not as stable as in the general population, so the skin is easily damaged. Depending on the location of the blisters, the disease can be divided into 3 main groups:
Simple epidermolysis bullosa: Caused by a defect in the gene encoding the keratin positions 5 and 15, the location of the blisters is in the epidermis. . Epidermolysis bullosa can continue: The bullous location is located at the junction of the epidermis and dermis, in the inner leaf layer. Epidermophytosis bullosa is caused by a defect in the gene coding for kallidin/laminin 5. The blister is located under the opaque leaf layer.

2. Symptoms of epidermolysis bullosa
Depending on the disease, the patient will have different clinical features:2.1. Simple bullous epidermophytosis Simple bullous epidermolysis bullosa consists of 17 different types, of which the most common are diffuse simple bullosa (Koebner) and focal simple epidermal detachment (Weber) -Cockayne):
Disseminated form: occurs in 1/50,000 newborn babies, sick immediately or after birth. After a few months, the disease will gradually ease and then recur when the baby can crawl or later. Manifestations of the disease are the regrowth of blisters, vesicles, and horny granules on the joints of the hands, elbows, and knees. The blisters usually do not leave deep scars. Lesions are usually more severe in the summer and milder in the winter. Usually no nail, tooth, or mucosal lesions or only mild lesions. Localized form: The most common form of the disease, the disease may not appear until adulthood, when the affected person participates in physical activities such as walking, marching, exercising excessively. Recurrence blisters on hands, feet, or superinfection, when healed, do not leave scars. Mucosal, nail no damage. The disease usually breaks out in the hot season.

2.3. Epidermolysis bullosa dystrophy There are subgroups as follows:
Dominant form:
Autosomal dominant dystrophy: Blisters and vesicles appear on extensor surfaces, especially joints of the toes and toes hands, knuckles, knees, elbows, ankles. Blisters may appear spontaneously without prior trauma. Milia usually appear on the face, ear lobes, backs of hands, extensors of forearms, and legs. Mucosal lesions, slippage in the oral mucosa, palate, tongue, pharynx, larynx,... Scars at the tip of the tongue, stunted hands, stiff storks, finger bone atrophy, pseudo-adhesion of fingers. Thick nails, dystrophy, hair loss, no hair. Teeth, eye conjunctiva without damage. Many patients as adults, the blisters gradually decrease, leaving only nail lesions. Transient bullous epidermolysis bullosa in infants: Blisters appear after any rubbing or even small transfer of substance. Usually heals quickly by 4 months of age. The nail has no damage, no scar.

Children get sick right after birth, blisters spread in the skin and mucous membranes. Fingers, toes stick into a wrap like a glove. Severe dental complications, uncontrolled spread of decayed teeth. Esophageal stenosis, anemia, malnutrition, mental retardation, risk of death from cardiomyopathy. High risk of developing squamous cell cancer
3. Diagnostic test for epidermolysis bullosa
In addition to the clinical signs, to diagnose the disease, the doctor must rely on the results of imaging techniques. The commonly used techniques are electron microscopy or immunofluorescence imaging. These techniques can identify epidermal cleavage and other defects such as hemidesmosome hypoplasia or loss of anchoring fibers.Blood samples or mucosal cells from a family member can be obtained for genetic analysis, the information of which can be used to develop gene therapy for the patient.
4. Treatment of epidermolysis bullosa
4.1.General principles of treatment Treatment depends on the severity of the disease and the degree of skin damage. Wound treatment, nutrition enhancement and superinfection prevention.4.2. Specific treatment Local treatment is the main treatment, including measures:
Avoiding trauma, care and treatment of infections. In case of skin lesions due to infection, give the patient systemic antibiotics. For simple disease: keep the patient in a cool environment, use soft, breathable footwear. Wash the blisters with saline, apply antibiotics, moist gauze. Patients often bathe with physiological saline, then apply moisturizer to protect the healthy skin. Skin graft surgery when indicated. For dystrophy: surgery to correct limbs, protect limbs from trauma, surgery to resolve spasticity around the mouth, perineum. In autosomal recessive dystrophy, patients often have squamous cell carcinoma, which must be surgically removed followed by radiation therapy. Comprehensive care is needed in critically ill patients with serial, multi-organ dystrophy. Improve nutrition, supplement iron. If the patient is constipated, eat a high-fiber diet and use stool softeners.

Previously used tetracycline, phenytoin, now use synthetic antimalarial drugs, steroids but in general the effect is not clear.
Protein therapy and gene therapy methods are having success in initial trials, opening a promising treatment direction in the future.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














