This is an automatically translated article.
The article was written by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalMedical imaging and colonoscopy play a very important role in diverticulitis of the colon, the means above not only help diagnose and evaluate the colonoscopy accurately, but also help guide treatment and treatment. treatment and monitoring progress.
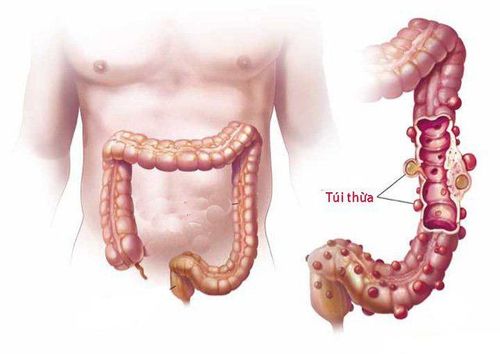
1.Contrast colonoscopy Contrast colonoscopy was once considered the gold standard for diagnosing colorectal cancer. The X-ray feature of diverticulum is a drug deposit originating from the wall of the colon.
The size of the diverticulum can vary from a few millimeters to a few centimeters. The lumen of the colon containing the diverticulum is often concentrically narrow, and the mucosa is serrated due to thickening of the sphincter and longitudinal muscles.
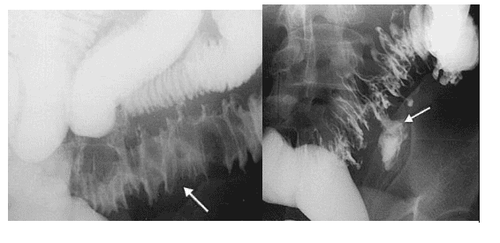
Chú thích ảnh trái: Mũi tên chỉ hình ảnh phù nề thành đại tràng trong VTTĐT Chú thích ảnh phải: Mũi tên chỉ ổ áp xe tạo ra do VTTĐT vỡ (Nguồn: Javier Casillas, trích từ Stollman N. và Raskin J.B. (2004), "Diverticular disease of the colon", Lancet, Vol.363 (9409), p.631-639)
However, according to pathogenesis, the inflammation of colonic diverticulum mainly occurs on the outside of the lumen of the digestive tract, while the CT scan only examines the inside of the colonic lumen, so the CT scan has less information. value.
In other words, scintigraphy only indicates the presence of a diverticulum, giving little information on the severity of the disease, especially in complicated diverticulitis. The rate of assessing the severity of VTE on contrast-enhanced radiographs is 41% lower than it actually is.
In UC, when the inflammatory process is progressing, angiography can still be performed but must use water-soluble contrast and not double-contrast (inflated and compressed). Electrocardiography with barium can cause peritonitis (VPM) and severe toxicity in cases where the diverticulum ruptures and barium escapes into the abdomen.
Inflating and compressing during double contrast imaging increases the pressure in the colonic lumen, causing the risk of perforation at the site of the inflamed diverticulum. With water-soluble contrast, the image of the contrast exiting the colonic lumen and flowing freely into the abdomen allows us to diagnose a ruptured diverticulum; Contrast images deposited in other organs such as bladder, vagina help diagnose gastrointestinal fistula complications.
Contraindicated to use high osmotic contrast in the case of patients in shock because the drug is hypertonic, which will aggravate the shock by reducing intravascular volume.
In summary, radiographs provide little information and are not very helpful in guiding treatment when diverticula are inflamed. However, after the acute inflammatory phase of about 4-6 weeks, dual-contrast barium scintigraphy is valuable in assessing the location and distribution of the diverticulum. Before taking the scan, it is necessary to prepare the phone to have a clearer image and to help thoroughly evaluate the entire colonic lumen to rule out other diseases.
2. Computed tomography (CT) CT has high sensitivity and specificity (97% and 100%), and a low false-positive rate. According to the American Society of Colorectal Surgeons, CT of the abdomen and pelvis is the most appropriate means to investigate suspected cases of colorectal cancer. CT provides a wealth of information for accurate diagnosis, detection of complications (abscess, gastrointestinal fistula, intestinal obstruction), assessment of the possibility of medical or surgical intervention, and monitoring of recovery.
Ambrosetti et al performed a study comparing CT and contrast angiography (with water-soluble contrast) in left CRC in 420 patients for 11 years. The results show that CT has a higher sensitivity than CT (98% versus 92%).
On the other hand, CT detected all UC patients with abscess complications in the study group, while contrast imaging only detected direct evidence of abscess (medication fossa with diverticulitis) in the study group. 29% of patients were in this group.
According to Rao, the accuracy of helical CT increases with the use of additional contrast agents (oral or transcolonic contrast, intravenous contrast). According to the same author, the sensitivity and specificity between routes of contrast administration are similar. However, intraluminal contrast injection has the advantages of being done quickly, reducing the time taken, avoiding discomfort, and reducing the rate of complications compared to oral or intravenous contrast.
The main criteria to diagnose diverticulitis on CT are:
Thickening of the wall (wall thickness ≥ 4mm) accounts for 70%. The diverticulum accounted for 84%. Change (increase) in the density of adipose tissue around the phone accounted for 98%. Abscess images (fossils of fluid around the cell) account for 35%.
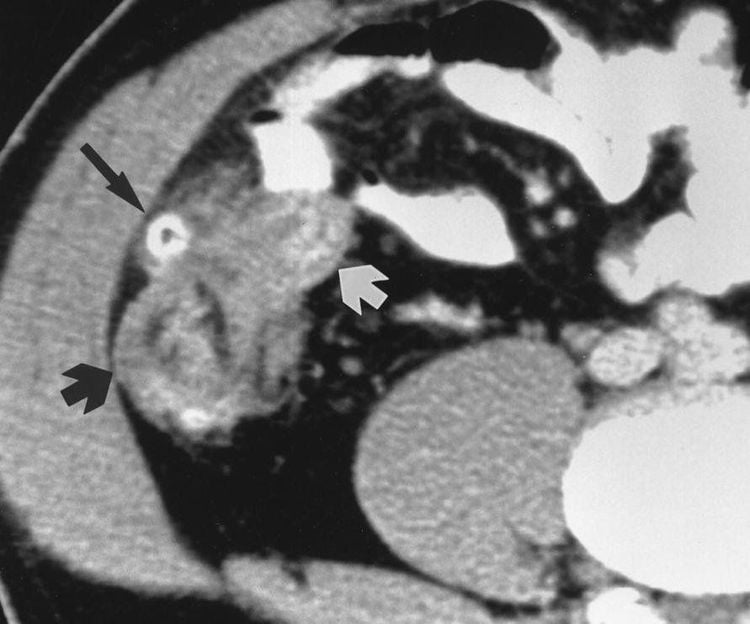
Hình ảnh CT của viêm túi thừa manh tràng (Nguồn: Jang H.J., et al. (2000), "Acute diverticulitis of the cecum and ascending colon: the value of thin-section helical CT findings in excluding colonic carcinoma", AJR Am J Roentgenol, Vol.174 (5), p.1397-1402)
Grade of diverticulitis on CT scan image:
Mild: sigmoid colon wall thickness <5mm, inflammatory reaction of pericolon adipose tissue Severe: Abscess, extraluminal gas CT detects accurately cases of UTI with complications such as VPM (image of fluid and diffuse inflammation), gastrointestinal fistulas (indirect images such as gas or contrast material from the colonic lumen deposited in the bladder, vagina, wall, etc.) abdomen; direct fistula images are rarely seen), and bowel obstruction (pictured with dilated loops of bowel with air and fluid, thickening of the colonic wall of the obstruction).
CT helps to accurately classify the disease according to the Hinchey scale in 90% of cases. Ambrosetti also provides a classification of the severity of CRC based on CT images. Accurate disease grading helps to select patients for conservative or surgical treatment. Conservative management of patients with severe diverticulitis has a high failure rate and an increased risk of secondary complications if treatment is unsuccessful.
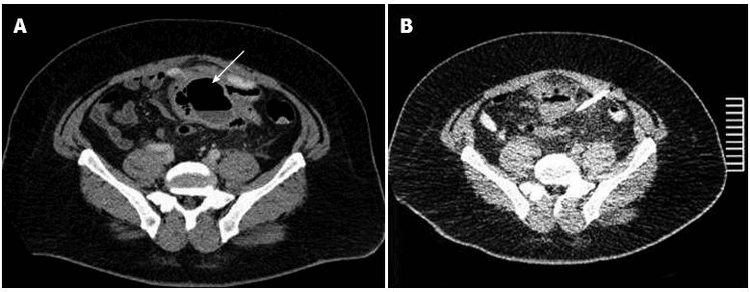
Hình A: Ổ áp xe do VTTĐT xích ma (mũi tên) Hình B: Ổ áp xe sau khi dẫn lưu một tuần (Mũi tên ODL) (Nguồn: Stocchi L. (2010), "Current indications and role of surgery in the management of sigmoid diverticulitis", World J Gastroenterol, Vol.16 (7), p.804-817)
In addition to the diagnostic role, CT also serves as a means of treatment. In VTE with large abscess complications, CT-guided percutaneous drainage of the abscess is performed to help drain the pus, reduce inflammation, and help the patient avoid an emergency surgery with the method of excision. , make an artificial anus (HMNT) and join in the second tense. After drainage and medical therapy for 2 to 4 weeks, the inflammation decreased and the patient was scheduled for surgery with the method of dialysis and one-stage anastomosis. With the above method, the patient only has to undergo one surgery instead of two and especially not emergency surgery. Therefore, patients will enjoy a lot of benefits while reducing costs and treatment time.
3. Magnetic Resonance Imaging (MRI) Colonic MRI is also a good imaging tool for evaluating colorectal cancer. This tool is useful in diagnosing right UTI and is a safe alternative to CT in the diagnosis and evaluation of UTI in young or pregnant patients.
MRI imaging in the diagnosis of colorectal cancer is based on the detection of at least one diverticulum, edema or effusion around the colon, and thickening of the wall. The use of high-resolution intravenous contrast in the T1 phase of MRI helps to diagnose complications of VTE with sensitivity and specificity equal to or higher than CT.
4. Colonoscopy

Túi thừa ĐT với hình ảnh sỏi phân bên trong

Túi thừa ĐT viêm: sung huyết niêm mạc lòng ĐT và mủ ở cổ túi thừa (Nguồn: Parra-Blanco (2006), "Colonic diverticular disease: pathophysiology and clinical picture", Digestion, Vol.73 Suppl 1 47-57)
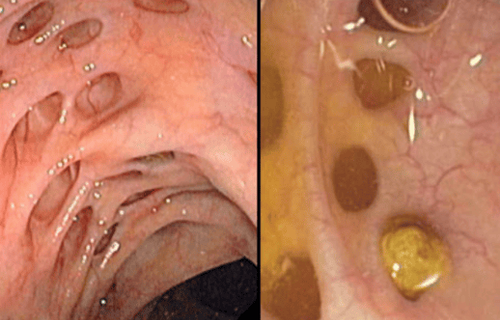
Hình ảnh nội soi đại tràng cho thấy đại tràng có nhiều túi thừa
Colonoscopy is very useful in the diagnosis of asymptomatic colonic diverticulosis and is an effective means of treatment in bleeding diverticula. However, in colonoscopy, endoscopic colonoscopy is considered a relative contraindication because the inflating process increases intraluminal pressure and may rupture the acutely inflamed diverticulum, causing VPM complications.
On the other hand, similar to CT scan, flexible bronchoscopy can only examine the inside of the colon, while the manifestation of colonoscopy mainly occurs on the outside of the gastrointestinal tract, so endoscopy does not provide much information for the diagnosis of VTE. However, endoscopic colonoscopy has a role in monitoring proliferative diseases after UTI treatment.
5. The role of ultrasound Ultrasound and CT are valuable imaging tools for colorectal cancer. Ultrasonography in the evaluation of VTE is increasingly widely used. Many studies have been carried out to detect the characteristic images and to evaluate the role of ultrasound in CRC.
Recent studies of ultrasonography on colorectal cancer aim to identify specific images to help differentiate right and acute VRT in order to improve the accuracy in diagnosis. The most common images in ultrasound are thickening of the wall of the colon, inflammatory response of the fatty tissue around the colon, and images of complications such as abscess, peritonitis.
Sometimes diverticulitis is present, but cannot be seen on ultrasound and CT Scan, we call it false negative. False negatives depend on many factors such as the diverticulum lying beyond the limit of investigation (deep lying), abdominal wall stiffness during examination, bowel gas, which limits the survey and the sonographer's qualifications.
For patients with lower quadrant abdominal pain, ultrasound should be performed, according to Oudenhoven, if a round or oval structure is detected that may originate from the right diaphysis but does not meet the criteria of VRT, it can be considered as image of diverticulum. This author also emphasizes the need to investigate and carefully evaluate the structure of the damaged segmental wall and the inflammatory images of the surrounding adipose tissue.
The criteria for the diagnosis of appendix are (1) in the lower right quadrant of the abdomen, on longitudinal section a “sausage”-shaped structure, terminal, non-peristaltic, and non-compressible, ( 2) on cross-section with characteristic target shape, and (3) diameter greater than 6mm.
To increase the sensitivity of ultrasound in right lower quadrant abdominal pain, the authors have given several guidelines:
Any small round or oval structure originating or adjacent to the umbilicus should be considered. to the diverticulum. The lumen of this structure may be low echo, empty echo, or thick echo. Inflammatory diverticulum may be surrounded by a layer of fluid (usually less than 3 cm) or surrounding fat. Kori describes the "dome" sign of the VTE on ultrasound as a poorly echogenic mass that protrudes from the outer surface of the wall. According to this study, this sign appeared in 100% of patients with right abdominal pain due to CRC. If there is no evidence of appendicitis, the diagnosis of right appendicitis should be considered and evidence should be sought. Although located near the appendix, the image between the diverticulum and the appendix is not difficult to distinguish, almost all appendixes are tubular whether located proximal or distal, while diverticula are round or oval. Combination of clinical and ultrasound symptoms.
6. Advantages and disadvantages of ultrasound and CT Scan in the diagnosis of colonic diverticulum Ultrasound has the advantages of being inexpensive, easy to apply, widely used, and has high sensitivity and specificity. However, the limitation of ultrasound is that it cannot investigate deeply, is hindered if there is a lot of gas in the intestine, the accuracy is highly dependent on the machine and the operator. In contrast, CT is a more objective means of assessment.
Common CT findings in colorectal cancer are colonic wall thickening, inflammation of surrounding fatty tissue, and diverticula. That image appeared at a rate of 70-100% in different studies.
Confocal wall thickening is a common and characteristic symptom of left rectal prolapse, and this image is also easily misdiagnosed with colonic neoplasms. The thickness of the colonic wall can help distinguish these two diseases, the wall in UC is usually concentrically thick and only about 1-3 cm thick, while in proliferative diseases the wall is often unevenly thick, and thickness greater than 3 cm.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of doctors, modern equipment and technology. The hospital provides comprehensive, professional medical examination, consultation and treatment services, a civilized, polite, safe and sterile medical examination and treatment space..
References:
Le Huy Luu, Nguyen Van Hai (2010), "Results of right colonic diverticulum surgery by laparoscopic surgery", Medicine of Ho Chi Minh City, volume 14 (additional to No. 4). ), p.12-15. Ly Minh Tung, Nguyen Van Hai (2011), Clinical features, images, and surgical results for diverticulitis. Aldoori W.H., Giovannucci E.L., Rockett H.R., et al. (1998), "A prospective study of dietary fiber types and symptomatic diverticular disease in men", J Nutr, Vol.128 (4), p.714-719. Ambrosetti P., Robert J.H., Witzig J.A., et al. (1994), "Acute left colonic diverticulitis: a prospective analysis of 226 consecutive cases", Surgery, Vol.115 (5), p.546-550.