This is an automatically translated article.
Article written by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International Hospital
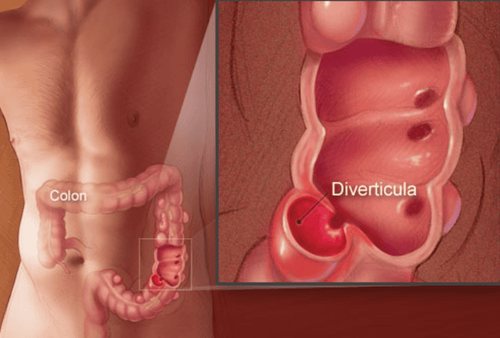
In terms of structure, the digestive tract is started from the mouth, esophagus, stomach, small intestine, large intestine, and finally the rectum and anus. The colon (also known as the large intestine) is the last and widest part of the digestive tract. Diverticulents are small, bulging pouches that can form anywhere in the digestive tract, from the stomach, small intestine, or large intestine, but are most commonly found in the colon.
Treatment of diverticulitis of the colon (DVT)
Oral antibiotics (outpatient)
Metronidazole combination + Fluoroquinolone or
+ Trimethoprim-sulfamethoxazole
Amoxicillin-clavulanate Intravenous antibiotics (hospitalization)
Combination therapy + Metronidazole or
+ Clindamycin
Combined with
+Aminoglycosides
+ Fluoroquinolones
+Third generation Cephalosporins
Second generation Cephalosporins Betalactam + betalactamase inhibitors Conservative treatment in patients with first UTI and no complications (class I according to the Society of Laparoscopic Surgery) Europe) has a success rate of 70-100%.
Patients who do not have high fever, do not have much vomiting, do not have signs of VPM and have follow-up conditions can be treated as outpatients. Outpatient treatment includes a liquid diet, oral broad-spectrum antibiotics, and antispasmodics. The antibiotic used must be effective against Gram-negative bacilli and anaerobic bacteria, commonly used is metronidazole in combination with fluoroquinolones. Other groups with good effects can also be substituted.
Close follow-up of outpatients is very important, symptoms should improve in 2-3 days. Patients continue to take antibiotics for 7-10 days. In the event that symptoms do not improve or there are other worsening events, the patient should be hospitalized.
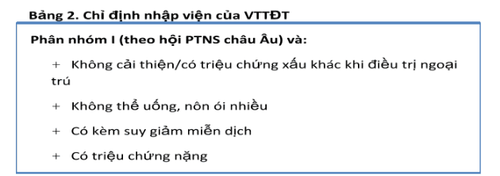
The medical treatment regimen for patients with indications for hospitalization includes bowel rest (oral discontinuation), feeding and intravenous antibiotics.
Recommended intravenous antibiotics are listed in Table 1. Patients can use analgesics, including hypnotics, but do not use morphine because they can increase sphincteric spasm and decrease peristalsis. intestine .
Usually, the disease will improve after 24-48 hours, manifested by the patient's abdominal pain, fever, abdominal pressure less pain and white blood cell count decreased. The patient was then switched to an equivalent oral antibiotic and the normal diet was gradually resumed from liquid to solid.
In case symptoms continue to not improve or worsen, surgery is indicated. A CT scan should also be performed when the patient is admitted to the hospital. CT helps confirm the diagnosis and assess the severity of the disease. The image of severe diverticulitis on CT according to Ambrosetti grade is a predictor of failure of medical treatment.
Patients after successful treatment should check and re-evaluate the entire colon with contrast-enhanced scintigraphy and colonoscopy to confirm the diagnosis and rule out other diseases such as colorectal cancer. , colitis .
The appropriate time is 6 weeks after medical treatment for the inflammatory process to be sorted out by the body. About one-third of patients after successful medical therapy will have recurrent episodes of diverticulitis, usually within the first year. A high-fiber diet helped 70% of patients avoid relapse for 5 years. Studies in Italy have shown that using mesalazine or rifaximin reduces symptoms and reduces relapse rates.
The percentage of patients requiring surgery in the group of patients admitted to the hospital for the first time because of UTI is 15-30%, most of them are in the group of patients with CRC with complications. With simple UTI, it is important to pay attention to patients with immunocompromised status, this group of patients has a higher rate of failure of medical treatment and a higher rate of complications.
For patients with a second episode of diverticulitis, medical treatment is controversial. The old view held that surgical intervention was needed in patients with a second episode of diverticulitis, the rationale being that the complication rate was increased by 60% and the mortality rate was doubled (compared to the first episode of diverticulitis). in this group of patients.
However, in 2002, Chautems, after following 83 cases of successful medical treatment for the first episode of UTI for 10.5 years, suggested that the recurrence rate was low and that medical treatment was still valuable in recurrent episodes of diverticulitis. The American Society of Colorectal Surgeons now recommends that the indication for surgery should be considered on a case-by-case basis.
Approximately 15% of patients with VTE have abscess complications. The diagnosis of an abscess is considered clinically (in the absence of CT) when a patient improves slowly with medical therapy or a tender, tender mass is palpable on the abdomen. These patients with UC with complications of this abscess should be hospitalized and given intravenous antibiotics. Treatment depends on the size and complexity of the abscess. Most small abscesses (≤ 2cm) can be resolved with medical therapy alone.

Larger abscesses are indicated for CT-guided percutaneous drainage. A resolved foci of infection results in a rapid improvement in symptoms within 72 hours and helps the patient avoid an emergency surgery (with colostomy, colostomy, and second phase anastomosis).
In patients with contraindications to surgery due to comorbidities, drainage may also alleviate symptoms and help better prepare the patient for an adequate follow-up. If the drainage tube (ODL) produces more than 500 mL of fluid in the first 24 hours, the diagnosis of gastrointestinal fistula should be considered. The drain is withdrawn when less than 10 mL of fluid remains in 24 hours.
It may take 30 days to achieve the above goal. Repeat CT scan with contrast agent injected through the ODL prior to withdrawal can help assess treatment outcome and detect anastomosis to the gastrointestinal tract. The most commonly chosen drainage site is the anterior abdominal wall. With deep pelvic abscess, during drainage treatment, the patient may have to lie on the stomach or side to drain the pus or have to drain through the rectum or vagina.
Drainage is only considered as 1 phase of the treatment process. The next stage was performed 3-4 weeks after successful drainage, the patient was scheduled for surgery with colectomy and one-stage anastomosis. With the above treatment method, the patient gets a lot of benefits:
No emergency surgery No need to wear an ostomy (Intestinal colostomy) Only one surgery (instead of two) should reduce the rate of complications. morbidity and mortality Reduction of treatment time and cost The success rate for drainage and elective surgery as above is 74-80%. Approximately 20-25% of patients with abscess complications require surgical treatment. Indications for surgery for the group of UTIs with abscess complications are multi-chamber or multifocal abscesses, which cannot be drained, or whose symptoms do not improve after drainage. Surgical resection and single-phase anastomosis for this group of patients is recommended, but not always feasible.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of doctors, modern equipment and technology. The hospital provides comprehensive, professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Le Huy Luu, Nguyen Van Hai (2010), "Results of right colonic diverticulum surgery by laparoscopic surgery", Medicine of Ho Chi Minh City, volume 14 (additional to no. 4), p.12-15. Ly Minh Tung, Nguyen Van Hai (2011), Clinical features, images, and surgical results for diverticulitis. Aldoori W.H., Giovannucci E.L., Rockett H.R., et al. (1998), "A prospective study of dietary fiber types and symptomatic diverticular disease in men", J Nutr, Vol.128 (4), p.714-719. Ambrosetti P., Robert J.H., Witzig J.A., et al. (1994), "Acute left colonic diverticulitis: a prospective analysis of 226 consecutive cases", Surgery, Vol.115 (5), p.546-550.