This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Esinophilic esophagitis is a chronic immune-mediated disease of the esophagus characterized by marked eosinophilic infiltration in response to type 2 (Th2) T helper cells. Factors such as genetics, environment, allergens, and gut microbiota have been identified as contributors to chronic disease.
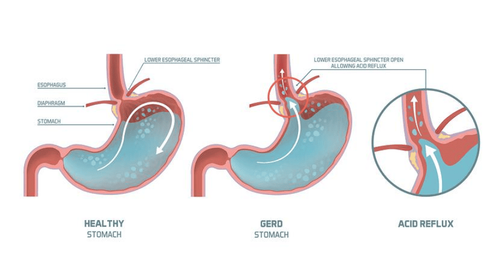
Dysbiosis is a term that includes a change in the composition of the combined microbiota compared with that found in healthy individuals. When differentiating the biome of a normal healthy esophagus from dysbiotic disease states, such as reflux esophagitis, esinophilic esophagitis, Barrett's esophagus, or adenocarcinoma of the esophagus, It is clear that biological dysregulation may precede inflammation. Gram-negative bacterial products activate Toll-like-receptors present on esophageal endothelial cells causing an inflammatory cascade, resulting in relaxation of the lower esophageal sphincter. Prevotella is found more frequently in dysbiosis distal esophagus, which has been shown to be a major producer of lipopolysaccharide, which contributes to Toll-like-receptor activation.
1. Eosinophil (Eosinophilic) esophagitis due to intestinal bacteria disorder
EoE is a chronic immune-mediated disease of the esophagus, characterized by marked eosinophilic infiltration in response to type 2 (Th2) T helper cells. Factors such as genetics, environment, allergens, and gut microbiota have been identified as causative agents of chronic disease.Several genes have been identified as contributing factors to EoE, including stromal lymphopoietin (TSLP), calpain 14 (CAPN14), esophageal microbiota SY, LRRC32, STAT6 and ANKRD27. Among the identified genes, TSLP appears to be the major contributor to this condition, as it is activated by epithelial cells and induces Th2 differentiation.
Various allergens also induce a wide range of symptoms that increase inflammatory markers, such as IL-5 and IL-13, creating a potential inflammatory pathway of EoE. In addition to genetic factors and environmental exposure, dysbacteriosis of the oesophagus has been implicated as a mediator in the pathogenesis of EoE.
2. The role of the microbiome
Microbiome analysis in EoE reported an increase in proteobacteria, especially Neisseria spp. and Corynebacterium spp., in children with active EoE. This study, combined with evidence of altered gut microbiota due to antibiotic use in neonates and cesarean delivery, further supports that dysbiosis in the human microbiome has a role in EoE .
Analysis by an esophageal sequence test to assess the microbiota of children and adults with active EoE showed greater abundance of Haemophilus spp. Notably, there was also a decrease in Clostridia-specific taxa in patients with active EoE. In antibiotic-treated mice, supplementation with a Clostridia-containing microbiome prevented sensitization to a specific food allergen. Induction of IL-22 by innate lymphoid cells, involving RAR receptors and T cells in the intestinal stroma, has been suggested as a blocking mechanism for food allergen sensitization. Recent evidence suggests that esophageal microbiota may be involved in the pathogenesis of EoE and represent new therapeutic approaches.
3. Conclusion
Esophageal microbiota plays a major role in the pathogenesis of esophageal disease. Disturbances in gut microbiota may contribute to a proinflammatory, cytokine-mediated state that begins in the submucosa. The pathogenic effect, which affects the lining of the esophagus, was previously thought to be caused by acid-induced mucosal damage, but now appears to be multifactorial, with esophageal microbiota playing a major role. Specific flora has recently been identified that may play a pathogenic role in this process.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: D'Souza SM, Houston K, Keenan L, Yoo BS, Parekh PJ, Johnson DA. Role of microbial dysbiosis in the pathogenesis of esophageal mucosal disease: A paradigm shift from acid to bacteria? World J Gastroenterol 2021; 27(18): 2054-2072 [DOI: 10.3748/wjg.v27.i18.2054]