This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Van Phan - Head of Interventional Imaging Unit - Department of Diagnostic Imaging and Nuclear Medicine - Vinmec Times City International General Hospital.Gastrointestinal varices are one of the causes of high gastrointestinal bleeding. This is one of the common complications in patients with portal hypertension syndrome. Currently, there are many methods to treat varicose veins, but the treatment by embolization method of gastric varices brings high efficiency, low recurrence rate and less invasiveness than other methods.
1. Percutaneous gastric varicose vein occlusion plug digitizes the background
Gastric varicocele embolization (BRTO) is an intravenous endovascular interventional technique, using a balloon-catheter, placed in the position of the left gastro-renal venous catheter, inflated. balloon to block this flow to avoid regurgitation, which then blocks all of the varicose veins communicating with the inferior vena cava system.1.1 Indications Gastric varices at risk of rupture: On endoscopic images, large dilated tufts, with focal points of congestion or ulceration, and rapidly progressed. Stomach varices ruptured: Repeated many times, endoscopy could not stop bleeding. Contraindicated with TIPS (portal anastomosis via jugular vein). An issue of note in the indications for BRTO is the case where the gastric vein is dilated and the left gastro-renal junction is present. In the absence of left gastric–renal venous junction, another route can be obtained, such as transhepatic access. 1.2 Contraindication Contraindicated Contraindicated Contrast allergy Renal failure: serum creatinine > 1.5 mg/dl Portal venous occlusion Severe, recurrent ascites due to portal hypertension Severe esophageal varices Women with pregnant.

2. The process of capturing and occluding gastric varicose veins through the skin digitized and erased the background
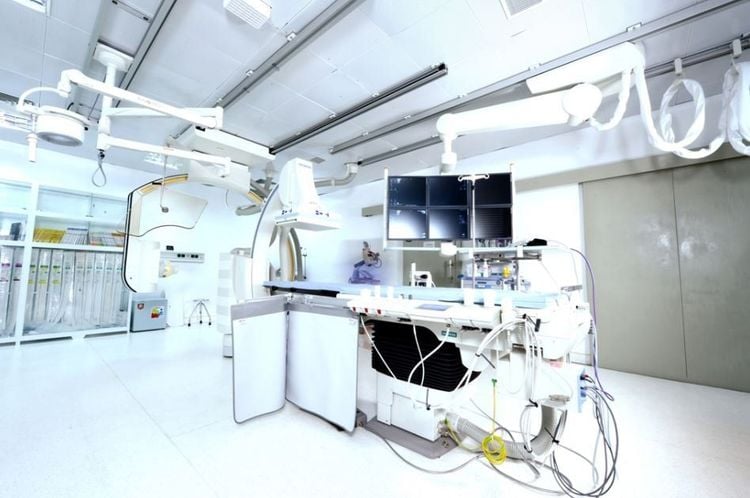
2.1 Preparations PerformerInterventional radiologist Interventional radiology technician Anesthesiologist/technician (if patient is difficult to cooperate) Nursing. Means of use:
Digital angiography eraser (DSA); Pacs image storage system; Specialized contrast injection machine; The lead skirt, shirt and collar help shield X-rays. Medicine:
Antiseptic solution for skin and mucous membranes. Local anesthetics General anesthetics (if needed) Water-soluble iodinated contrast agents; Heparin and Heparin neutralizing drugs; General medical supplies:
Syringe 1, 3, 5, 10, 20ml and pump for contrast injector. Physiological saline; Etroley cars; Surgical clothing; Sterile kit (scissors, knife, tongs, tool tray, etc.); Cotton gauze, surgical medical adhesive tape. Special medical supplies:
Arteriocentesis needle; Standard conductor 0.035 inch; Long sheath 6F - 12F; Microcatheter 1.9F-2.7F, microwire 0.014-0.018 inch; Catheter with balloon - catheter.
Bio-foam to help stop bleeding; Metal coils (coils) of all sizes; The embolic agent sclerosant; Bio-adhesive (Histoacryl); Patients need to prepare:
Be explained carefully about the procedure to coordinate with the doctor; Clinical examination before the procedure; Fasting before 6 hours, do not drink more than 50ml of water; If the patient cannot lie still, sedation will be prescribed. Test sheet:
Medical record for inpatient treatment There is a written order to perform the procedure approved by X-ray, computed tomography, magnetic resonance imaging (if any). 2.2 Procedures Intravascular access
Local anesthesia, skin incision. Inject the lumen (right common femoral vein, right internal jugular vein) under ultrasound guidance. Routine insertion of catheters Angiography to assess lesions
Use catheters and leads to access the left renal vein and the site of the gastrorenal shunt (gastrorenal shunt). Insert a balloon catheter (Forgarty catheter) into the gastro-renal vein. Perform balloon inflation to completely block the flow of this venous anastomosis. Perform angiography of varicose veins of the stomach through a balloon catheter. Evaluation of the entire system of varicose veins and collateral branches, drainage. Embolization of the collateral branches
Use a microcatheter and a microguide wire to access the branches of the collateral veins Perform occlusion of these collateral veins with a metal coil (Coils) ).
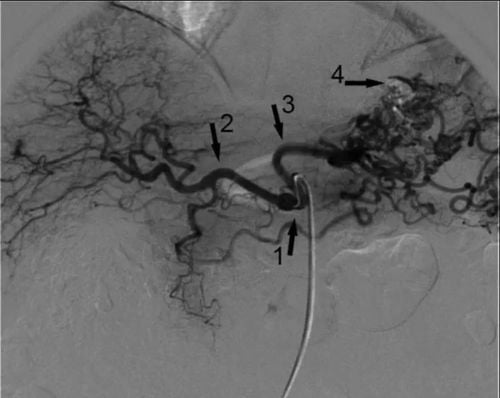
The balloon catheter remains in the left gastro-renal vein, the balloon is inflated until the venous flow is completely blocked. Insert the microcatheter into the varicose vein through the balloon catheter. Inject sclerosing, embolizing agent into varicose veins through microcatheter. Lock the microcatheter and balloon catheter to prevent reflux of fibrous substances. Monitor and evaluate
Take the patient back to the ward with the catheter, the microcatheter locked and still in the vessel After 4-24 hours, take a CT scan of the abdomen with contrast injection to assess the level Obstruction of varicose veins of the stomach. End of procedure
When varicose veins are blocked according to the results of abdominal CT scan, take the patient back to the intervention room. Angiography to check the degree of obstruction through the microcatheter. Withdraw the entire catheter, microcatheter. Close the vascular access, end the procedure. BRTO is successful when the entire dilated gastric varices have collapsed due to fibrosis, thrombosis, no longer enhanced on CT images. The branches no longer flow.
3. Accidents and handling
3.1 Portal hypertensionOccurs about 15-27% after 1 year and 45-58% after 3 years. Consequences of portal hypertension can lead to rupture of esophageal varices and increased levels of ascites.
3.2 Acute renal failure When there is acute renal failure, it is necessary to consult a nephrologist - urologist to manage renal failure.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.