1. What is uterine prolapse?
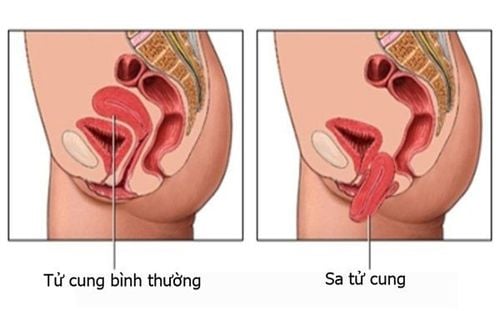
Uterine prolapse refers to the descent of the uterus into the vaginal canal or, in severe cases, its protrusion outside the vagina. This condition occurs when the pelvic ligaments and muscles become stretched or weakened, losing their ability to adequately support the uterus.
2. Degrees of uterine prolapse
Grade 1: The uterus descends but remains within the vagina.
Grade 2: The uterus partially protrudes out of the vagina, but the body of the uterus is still attached.
Grade 3: The uterus completely protrudes outside the vagina and can be observed with the naked eye. At this stage, it becomes very dangerous and may require a hysterectomy due to infection risks.
3. Signs of Uterine Prolapse
Here are the common symptoms of uterine prolapse:
- Difficulty and pain during urination.
- Lower back pain when lifting objects, abdominal discomfort, inability to suck in the abdomen, and a constant feeling of fullness in the belly.
- Vaginal pain or burning sensation during intercourse.
- The uterus protrudes outside the vagina, making sitting and walking difficult.
- A sensation of sitting on a ball or feeling as though something is about to fall out of the vagina.
Whether uterine prolapse is hereditary or congenital is not the main concern. The most important thing is how to effectively treat this condition.
4. Can congenital uterine prolapse affect pregnancy?
If you have stage 1 uterine prolapse, you can still get pregnant, but it is essential to consult your doctor. The best advice is to treat the condition completely before trying to conceive.
Pregnancy with uterine prolapse presents challenges in maintaining the pregnancy, increasing the need for close monitoring. Normally, pregnant women have check-ups every 4 weeks, but for those with uterine prolapse, check-ups every 2 weeks are recommended.
To closely monitor the baby's condition, you should see a doctor immediately if frequent contractions occur. Whether you give birth naturally or by cesarean section will depend on the health of both the mother and the baby, so early prenatal care is critical.
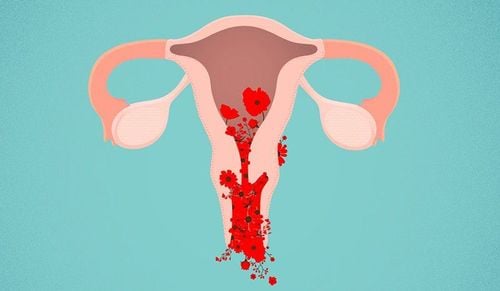
If the condition progresses to stage 2 or 3, where the uterus has descended below the vagina, there is no longer enough space for the fetus to develop. This may lead to fetal demise. In severe cases, the fetus might be expelled before it is fully developed, causing stillbirth, birth defects, or increasing the risk of postpartum hemorrhage for the mother.
Additionally, complications such as urethral, bladder, or rectal prolapse may occur. If left untreated, the condition may result in severe infection or loss of the uterus's natural elasticity, leading to a hysterectomy (removal of the uterus).

5. What causes uterine prolapse?
5.1 Objective causes
- Congenitally, the pelvic bone structure is larger than normal.
- Uterine malformations or abnormal shapes.
- During pregnancy, taking certain medications with strong side effects can affect the baby’s development in the womb.
5.2 Subjective causes
- Having multiple pregnancies or frequent premature births.
- Unsafe abortions at unreliable clinics, which damage the uterus's elasticity.
- Early sexual activity before the uterus has fully matured.
- Pregnancy with a large baby while the mother’s health is weak.
- Performing heavy labor or maintaining long, strenuous positions that put pressure on the abdomen.
- Lack of a balanced diet and scientific nutrition. Mental stress, anxiety, or nervousness can also contribute to the condition.
6. Treatment and Prevention
6.1 Preventive measures
To prevent uterine prolapse, individuals should practice the following:
- Engage in pelvic floor strengthening exercises to improve flexibility and endurance. Recommended exercises include Kegel exercises, pelvic stretches, and core-strengthening activities such as sit-ups.

- Have regular health check-ups to detect the condition early and receive appropriate treatment.
- Avoid heavy lifting and refrain from taking medications with strong stimulatory effects
- For abortion procedures, visit safe and reliable medical facilities to prevent the disease and avoid recurrence.
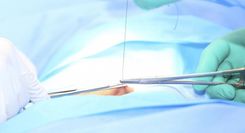
6.2 Treatment for Uterine Prolapse During Pregnancy
- For pregnant women with uterine prolapse, adhering strictly to a doctor-recommended exercise regimen is crucial for managing symptoms and ensuring a safe pregnancy.
- Clean the genital area properly to prevent infection of the prolapsed uterus.
- Some herbal medicines that are safe for both the mother and baby can be used to improve uterine elasticity, making childbirth easier. However, the dosage must be taken as prescribed by the doctor.
- Follow a healthy and balanced diet by eating plenty of vegetables and fruits, drinking lots of water, and limiting dry foods and fast food.

At Vinmec International General Hospital, the BASIC GYNECOLOGICAL EXAMINATION AND SCREENING PACKAGE is now available. This package helps customers detect gynecological infections early, making treatment easier and more cost-effective. Additionally, it allows for early screening and detection of gynecological cancers (such as cervical cancer) even before symptoms appear.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.