This is an automatically translated article.
The article was written by Specialist Doctor II Pham Tien Ngoc - Emergency Resuscitation Department - Vinmec Central Park International General Hospital
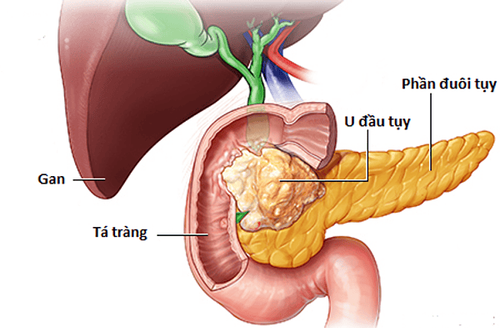
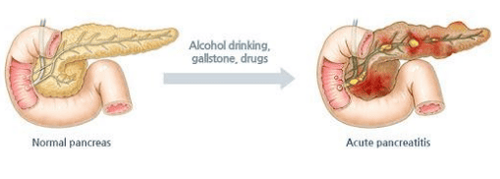
Acute pancreatitis (VTC) is a common medical and surgical emergency. Most of the symptoms of acute pancreatitis are mild, can be self-reversible (80-85%), the remaining 15-20% can progress to severe with serious complications, high mortality rate (up to 15%). 30-40%). Some cases initially presented with mild acute pancreatitis but then progressed to severe acute pancreatitis leading to shock, sepsis, multi-organ failure and death.
Therefore, the initial assessment and prognosis of the patient's severe course are extremely important to help detect serious complications early and thereby have immediate interventions to reduce the mortality rate for patients. patient.
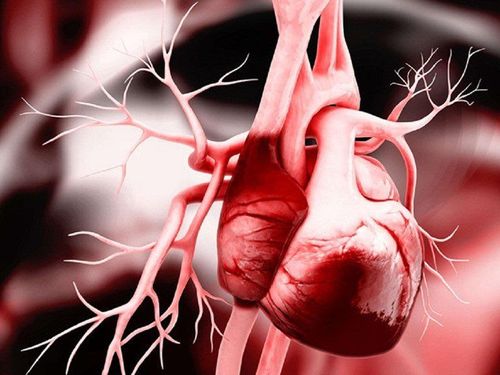
Viêm tụy cấp
1.The scale to assess the degree of acute pancreatitis
There are many scales to assess the severity of VTC such as: Ranson criteria, APACHE II prognostic table, Imrie score (improved Glasgow), Balthazar scale, BISAP,...
These scales have been evaluated. widely used for many years but still reveals many limitations. For example, the Ranson criterion is the most commonly used scale to date, but is evaluated at the first 48 hours of admission, to collect all necessary tests.
Therefore, can lead to severe delayed treatment of VTC. As for the APACHE II prognostic table, although it can be evaluated at any time, it requires many complicated calculation parameters and is difficult to remember, so it is less common in clinical practice.
Particularly with the Balthazar scale, the assessment of prognosis requires to be based on the results of computed tomography; Therefore, it requires high-tech equipment, expensive costs, and moreover, computed tomography should only be performed at least 48-72 hours after the onset of the disease to clarify the image of pancreatic necrosis. (if any) so it is not applicable to all patients.
2. Japanese severity score (JSS)
The Japanese severity score (JSS) has been applied in Japan since 1990 (suggested by the Japanese Committee for Pancreatic Pathology Research) to predict the severity of pancreatitis.
Scale includes 5 clinical signs, SIRS, age, 10 paraclinical parameters and computed tomography. Divided into 5 degrees (0-4), the total score is 27 points and is considered severe when the JSS is ≥ 2 points. According to the study of author Rawad M, in 2012, the sensitivity and specificity of the JSS scale were (59% and 92%), respectively, positive predictive value (70%) and negative predictive value. (88%).
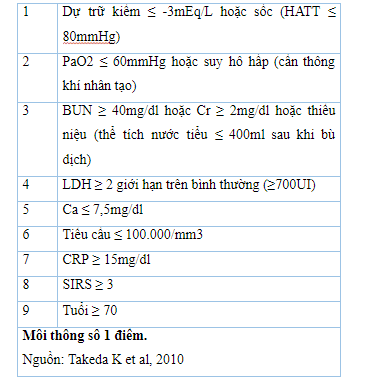
Since 2008, the JSS scale has been improved with 9 parameters, each parameter 1 point, is considered heavy when JSS improves ≥ 3 points:
Author Pham Tien Ngoc, studied the value of the JSS score on 148 patients with acute respiratory syndrome hospitalized at Gia Dinh People's Hospital from May 2015 to May 2016, drawing the following conclusions:
JSS score ≥ 3 statistically significant association with the risk of severe acute pancreatitis (p < 0.001). In the prognosis of severe acute pancreatitis according to the 2012 Atlanta criteria, with the JSS index ≥ 3, the sensitivity is 100%, the specificity is 84.17%, the positive predictive value is 29.03%, the predictive value is negative 100%, the area under the curve is 0.969. The JSS, BISAP and Ranson scales all have equally good predictive ability of severe VT, with the area under the ROC curve being 0.969, 0.929 and 0.928, respectively. With a diagnostic threshold of 3 points, all 4 scales have similar specificity, positive predictive value and negative predictive value in the prognosis of severe VT. However, the JSS score has the highest sensitivity (100%), followed by BISAP (88.89%), third Ranson (77.78%) and finally Imrie (44.44%).
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.