This is an automatically translated article.
The article was written by MSc Bui Thi Hong Khang - Pathologist, Laboratory Department - Vinmec Central Park International General Hospital.Laboratory Pathology (Hitology), also known as biopsies, are tissue samples taken from living people for diagnostic and therapeutic purposes. Test Cytology is another type of material that can be taken from a living person to examine the pathology of the cell types found in body fluids (pleural fluid, peritoneal fluid, urine), or cells. spontaneous sloughing from the various types of covering epithelium (vaginal-cervical epithelium, bronchial epithelium).
1. Pathological examination (Hitology)
Tissue samples can be removed in several ways (Figure 1):
Surgery : a sample of tissue, part or all of a diseased organ is removed surgically. Examples: part of the cervical lymph nodes, the entire stomach, a lobe of the thyroid gland. Endoscopic biopsy: Using an endoscope, a small piece of tissue can be cut with forceps deep in the digestive tract, respiratory tract, or urinary tract. Core needle biopsy: thanks to special needles, a small sample of breast tissue, liver, kidney, pleura or bone marrow can be obtained... Immediate biopsy (cold cut): helps to quickly identify the tumor is benign or malignant right at the time of surgery, so that the surgeon will give appropriate treatment directions for the patient. Fine needle aspiration biopsy (FNA or FNAB: fine needle aspiration biopsy)
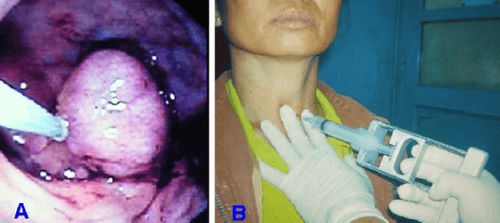
Hình 1: Sinh thiết polýp đại tràng qua nội soi (A); sinh thiết chọc hút bằng kim nhỏ (B)
We can also aspirate cells of any organ in the body with a fine needle (size 23-24). This test has high sensitivity and specificity in the diagnosis of papillary thyroid carcinoma.
Biopsy: surgical, or endoscopic Immediate biopsy (cold biopsy) Core biopsy (FNA) Fine-needle aspiration biopsy
2. Cytological examination
This is a test for PAP , Thinprep, or peritoneal, pericardial, pleural, bronchoalveolar lavage...
Cervical vaginal smear (PAP, Thin Prep) Nipple discharge Body fluid such as peritoneum, pleura...
3. Cell block
Cell Block: Peritoneal and pleural fluid, when suspected of having metastatic malignant cells, in addition to direct smear to observe cells, can also be centrifuged to get sediment and buried candles. This technique allows the deposit to be treated as a tissue sample and to perform other techniques such as a GPB tissue sample.
Diagnostic aids in GFB testing:
3.1 Special staining: (histochemistry) Giemsa for Helicobacter Pylorii PAS staining Trichrome staining Gomori reticulin reticulum staining (silver staining) 3.2 Immunohistochemical staining Diagnosis of kidney diseases and kidney transplant rejection. Determine the origin of malignant cells. Support in choosing treatment methods and assessing prognosis for cancer patients: + Endocrine or targeted therapy in breast cancer: ER, PR, Her2/ Neu
+ Immunotherapy: PDL1
+ Prognosis and individualization of treatment: MMR (MLH1, MSH2, MSH6, PMS2)
FISH in situ hybridization for Her2/Neu mutations HMMD Dual-ISH Her2/Neu staining Gene sequencing detect gene mutations: EGFR, KRAS, BRAF, ALK1, ROS1...
4. How is pathological examination performed?
Tissue samples removed from the body must be fixed and processed to observe pathological images on a microscope, including the following steps:
Fixation: When the surgical tissue or organ sample is removed from the body will be fixed immediately in 10% formaldehyde to keep the cells and tissues as they were alive in the body to ensure that the pathological damage is not changed. Macroscopic observation and selection of the pathology location, resection and tissue treatment: This fixed tissue or organ sample will be sent to GPB laboratory to be observed by GPB doctor with the naked eye and recorded. on the test sheet of the specimen, even recording all the morphological features (such as size, color, density, limit, envelope...) of the pathological tissue. Then proceed to select the location of the lesion, cut the characteristic sample, take it to process the tissue through many chemicals so that it can finally be cut to 1-3μm thin to be able to observe the cells on the microscope. Microscopic and ultra-microscopic observations: After being thinly sliced and stained, the specimen will be studied for cell and tissue lesions under an optical microscope or an electron microscope. To be observed under the optical microscope, the tissue sample must be fixed, processed, thinned and stained, the preparation time takes about 3-4 days. Specimens with bones need to take 2-3 more days to decalcify the bones before they can be thinned. Microscopic observation requires tissue samples to be cut as thin as 0.1 μm, the preparation time takes months, so it has little applicability in routine pathological diagnosis, mainly for research purposes. .
5. Why are other techniques needed to aid the diagnosis in GPB tests?
5.1 Special staining In order to visualize the lesions present in cells and tissues, staining is required for easy visualization. The routine staining method in the pathology laboratories is the Hematoxylin-Eosin staining method: the cells will have purple nuclei and the cytoplasm will be pink (Figure 2A).
In some cases, additional histochemical staining methods (also known as special staining) can be used to identify certain structures of cells and tissues based on their particular affinity for certain types. some chemical. For example, Giemsa staining for Helicobacter Pylori bacteria, PAS staining to detect glycogen and mucus in cells, Trichrome staining to clearly see collagen fibers. Used to diagnose cirrhosis or kidney diseases (Figure 2B,C). ).
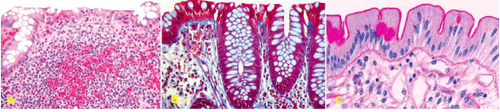
Hình 2: Niêm mạc đại tràng nhuộm Hematoxylin-Eosin (A); nhuộm Trichrome, thấy rõ màng đáy bắt màu xanh dương; nhuộm PAS (periodic acid-Schiff), giọt chất nhầy của tế bào đài bắt màu hồng.
5.2 Immunohistochemistry Recently, immunohistochemical staining technique has been widely applied in pathology laboratories in HCMC to aid in diagnosis. This is a special staining technique that uses an antigen-antibody combination reaction to detect structural components (antigens) present in cells and tissues. The antigen - antibody binding site will be visualized by the reagents . (Figure 3). Depending on the chemical displayed, two main immunohistochemical staining methods are distinguished:
* Immunofluorescence:
Antibodies are bound to fluorescein. If there is an antigen-antibody reaction (that is, the presence of the antigen of interest in the tissue sample), the antigen-antibody complex will fluoresce when stimulated by ultraviolet light, observed under fluorescence microscope. Fluorescence can be directly attached to specific antibodies, called direct immunofluorescence; or bind to a second antibody specific to the first, called indirect immunofluorescence. Immunofluorescence is used mainly in the diagnosis of glomerular and some skin diseases (Figure 4A).
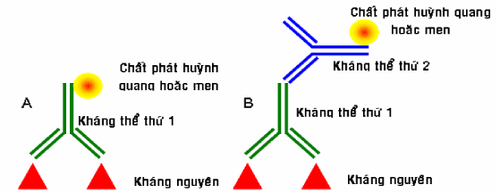
Hình 4: Miễn dịch huỳnh quang và miễn dịch men, trực tiếp (A) và gián tiếp (B)
* Enzyme immunity:
Antibodies are bound to enzymes (enzymes). When chromogen is added to the tissue sample, the yeast precipitates the pigment (usually brown) at the site of the antigen-antibody complex, making it visible under the light microscope.
As with fluorescein, if yeast is directly attached to the first antigen-specific antibody, it is called direct enzyme immunoassay. When the enzyme is attached to a second antibody specific to the first, it is called indirect enzyme immunity.
Enzyme immunoassays are widely used in the diagnosis of tumor diseases:
Help determine the origin of tumors that are too poorly differentiated or undifferentiated to differentiate between carcinomas, sarcomas, or lymphomas (Figure 19B). . Help evaluate prognosis and response to treatment: Assess the status of estrogen receptors, progesterone, Her-2/neu receptors for breast cancer.
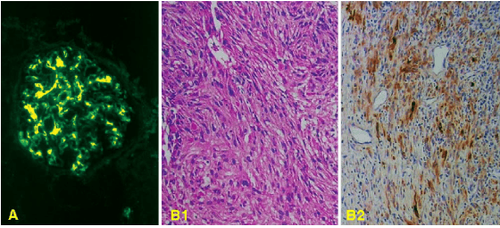
Hình 4: Hoá mô miễn dịch huỳnh quang, dùng kháng thể huỳnh quang chống IgA cho thấy có sự lắng đọng của IgA ở vùng giãn mao mạch trong bệnh thận IgA (A). Một u kém biệt hoá cấu tạo bởi tế bào hình thoi trông giống như một sarcoma (B1), nhuộm hóa mô miễn dịch men với kháng thể chống cytokeratin cho thấy tế bào u bắt màu nâu (B2), chứng tỏ đây là một carcinôm chứ không phải là sarcoma.
Provides valuable information for prognosis and individualization of treatment:
+ HMMD staining to detect PDL1 mutations in cancer cells is used to predict patient response to therapy. immunotherapy.
+ HMMD staining of the protein quartet of the MMR DNA mismatch repair genome (MLH1, MSH2, MSH6, PMS2) not only to screen for Lynch syndrome but also to help differentiate between colorectal cancers lacking the repair system deficient mismatch repair (dMMR) with satellite-stable colorectal cancer (MSS). These two types have different prognosis and response to treatment.
FISH AND DUAL-ISH HER2/NEU:
In addition, advanced techniques applying molecular biology such as fluorescent in situ hybridization (FISH), etc. are also gradually being used in the pathology laboratory for diagnostic work. For example, in the HMMD Her2/Neu staining field it is not clear whether redefining by FISH or Dual-ISH is supported. (Figure 5).
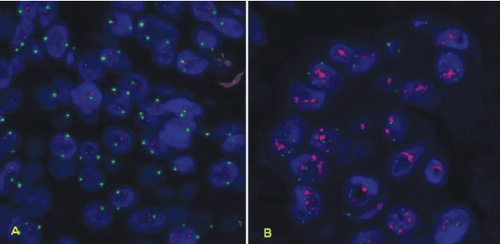
Hình 5: Kỹ thuật FISH cho thấy có sự khuyếch đại gen HER-2/neu lên gấp 3 lần (biểu hiện bằng các đốm đỏ trong nhân) ở các tế bào carcinôm tuyến vú (B) so với tế bào biểu mô ống tuyến vú bình thường (A).
Molecular biology: Polymerase chain reaction (PCR)
As for molecular biomarkers, many genes involved in cell signaling pathways are mutated in lung cancer such as KRAS (mutation rate 15-25%), EGFR (10-35%), ALK (3-7%), HER2 (2-4%), MET (1-2%), ROS-1 (1 -2%),...
Molecular biology tests have a particularly important role in the selection of treatment regimens, prognosis, and monitoring of treatment with targeted drugs. Among them, testing for EGFR mutations and ALK translocations is the most meaningful in clinical practice.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.
Reference materials GPB Textbook GPB Department of Medical University Pham Ngoc Thach HCMC.














