This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
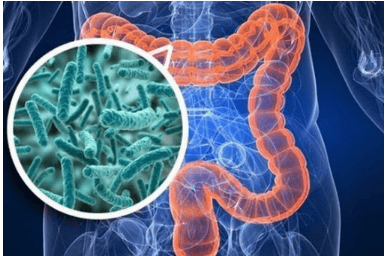
Many microorganisms play a role in gut health; they include bacteria, fungi, and viruses that exist in dynamic equilibrium to maintain mucosal homeostasis. Disturbances in the gut microbiota disrupt mucosal homeostasis and are strongly associated with inflammatory bowel disease (IBD) in humans and colitis in mice. Therefore, preventing or correcting microbiome imbalance can be considered as a new prevention or treatment strategy for IBD.
1. Probiotics: Live Bacterial Biological Therapy
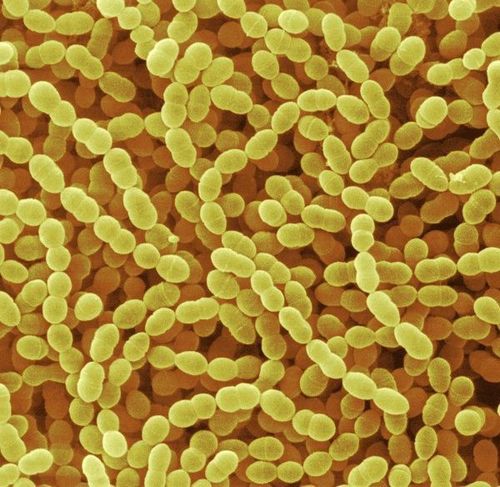
Probiotics were first proposed in 1908 by Nobel laureate Eile Metchnikoff, who also identified the first probiotic agents, lactic acid bacteria, to have the physiological effect of inhibiting “autotoxicity processes.” intestine", slows down the aging process of the intestine and produces beneficial effects on human health. Since then, the concept of gut probiotics has been constantly evolving and new strains of beneficial bacteria are still being identified. The latest scientific definition of probiotics, i.e. . “Living microorganisms, when used in adequate amounts, confer a health benefit to the host” was raised in 2014. The probiotic strains discovered so far mostly belong to the Firmicutes group and include genera Aerococcus, Enterococcus, Lactobacillus, Lactococcus, Leuconostoc, Oenococcus, Pediococcus, Streptococcus, Carnobacterium, Tetragenococcus, Vagococcus and Weissella; as well as the genera Bifidobacterium due to Actinobacteria and Saccharomyces belonging to Eumycota. Lactobacillus, Bifidobacterium and Saccharomyces are probiotics with a long history of application and are of great interest to many people. Furthermore, with evolution and innovation in sequencing technology, researchers have discovered new probiotic strains known as “next generation probiotics”, including Akkermansia muciniphila, Propionibacterium spp. And Roseburia spp., with promising applications.2. Clinical Application of Probiotics
The clinical application of probiotic preparations is still very limited, their scope of application and effectiveness are still being studied. As a blend of high-concentration probiotic preparations, VSL
3 consists of 8 live lyophilized strains of bacteria, namely Streptococcus thermophilus, 3 strains of Bifidobacteria (B. longum, B. breve, and B. infantis) and 4 strains of Lactobacilli ( L. paracasei , L. plantarum , L. acidophilus and L. delbrueckii subspecies bulgaricus ). VSL
3 has long been used in clinical settings for the treatment and remission of IBD. One study confirmed that VSL
3 achieved remission in patients with mild to moderate active UC, with high safety and efficacy.
Furthermore, in a recent systematic meta-analysis, VSL
3 also demonstrated efficacy in reducing UC active and pouchitis, and may effectively protect against its recurrence in static disease stage; however, its potential use in CD patients has not been demonstrated. The exact effects of probiotics in the gut are still unclear.
3. The impact of probiotics on the gut
The elucidation of the mechanisms by which probiotic bacteria exert a protective effect in IBD is important for determining optimal treatment strategies. The potential effects of probiotics on the gut can be classified into 4 categories:
(1) Probiotics modulate immune responses and inhibit inflammatory responses by mediating several signaling pathways. signaling, such as the Toll receptor-like signaling pathway;
(2) Probiotics directly inhibit or eliminate intestinal pathogenic microorganisms by competing for nutrients and intestinal epithelial adhesion sites, and secreting antimicrobial substances;
(3) Probiotics help maintain intestinal epithelial homeostasis by promoting tight junction (TJ) formation, promoting mucus production, and resisting epithelial cell death;
(4) Probiotics can directly affect the metabolism of the intestinal microbiota and the host, thereby promoting the regulation of colon cell proliferation and elimination of toxic substances. out of the intestine.
Diverse antibiotic mechanisms and agents are involved, e.g. lactic acid can disrupt gut microbiota metabolism by lowering pH, bacteria can damage growth cytoplasmic membrane formation, and bacteria disrupt macromolecule synthesis pathways. An antibacterial protease encoded by Lactobacillus paracasei partP, lactocepin, can selectively degrade IP-10 levels of the anti-inflammatory chemokine.
4. Prebiotics: Nourishing probiotic preparations
Indigestible oligosaccharides, especially fructo-oligosaccharides, have long been used to promote health. Prebiotics were first defined as a “non-digestible food ingredient that beneficially affects the host by selectively stimulating the growth and/or activity of one or a limited number of microorganisms.” colonized bacteria” in 1995. Since then and especially from 2001 to 2014, the concept and meaning of prebiotics has expanded; The latest and most widely accepted definition is “substrate selectively used by host microorganisms to confer health benefits”. A large class of prebiotics are oligosaccharides, including cereal-derived arabinoxylans and arabinoxylans, fructo-oligosaccharides (FOS), galacto-oligosaccharides (GOS), glucans, glucose/xylo-oligosaccharides, isomalto-oligosaccharides, poly-dextrose, oligosaccharides soybeans, and trans-galacto-oligosaccharides.

5. Effects of Prebiotics
The effect of prebiotics is to stimulate certain groups of microorganisms, and to increase not only the abundance of Lactobacillus and/or Bifidobacterium but also other beneficial taxa, such as Roseburia, Eubacterium and Faecalibacterium spp. . A recent study showed that inulin induces alterations in the gut microbiota, manifested in an increase in the abundance of Bifidobacterium and Anaerotipes, and a decrease in the abundance of Bilophila.
Prebiotics promote the propagation and growth of probiotics, whose metabolites confer health benefits to the host. For example, some organic acids are major metabolites produced by the metabolism of prebiotics by the host microorganism. The main organic acids produced are short-chain fatty acids (SCFAs) (eg, acetate, butyrate, and propionate), which directly lower the pH in the colon; In addition, SCFAs may mediate multiple signaling pathways to maintain intestinal homeostasis and immune system.
FMT (fecal bacteria transplantation)
FMT is the transfer of fecal microorganisms from healthy donors to individuals with certain diseases, through technical methods such as douching , nasogastric or nasojejunal catheter, and oral capsule. FMT was first used to treat pseudomembranous enterocolitis (PMC) in 1958, by Eiseman et al. Subsequent studies have suggested that PMC is caused by infection with the anaerobic bacteria C.difficile, which can cause intestinal dysbiosis. FMT has since been gradually expanded from the preliminary stages of development and testing to be used as an approved treatment modality for C.difficile infection (CDI) in the clinic, with success rates. close to 92%, thus representing an effective treatment compared to broad-spectrum antibiotics. Later, FMT was used to treat IBD complicated by CDI, and was eventually extended to treat patients with IBD only. As a treatment strategy for IBD, FMT has been proposed for more than 25 years. five; however, it has only attracted research interest in the context of IBD in recent years. Several clinical studies have demonstrated promising therapeutic results for patients in the mildly or moderately active phase of the disease.
6. Herbal Compounds and Prescriptions
There are some safety concerns with long-term use of common drugs (e.g. anti-inflammatory, immunosuppressive and biologic therapies), which has increased interest in these drugs. Traditional medicine to treat IBD. As a result, more and more researchers are turning their attention to traditional medicine to identify potentially curative compounds in Chinese herbal medicine and/or traditional prescriptions.
To date, various potent compounds have been found, some of which exhibit an effect on reducing intestinal inflammation, at least in part by modulating the gut microbiota. However, the meager data may actually reflect the treatment's effectiveness in human clinical trials. Many types of natural compounds are derived from herbs, including herbal polysaccharides, polyphenols, flavonoids, saponins, and alkaloids. Furthermore, herbal polysaccharides and polyphenols, which are present in various Chinese herbs and are almost exclusively absorbed in the colon, have not yet been included in the prebiotic category. Herbs containing polysaccharides include several Chinese medicines such as American ginseng and wild wolfberry, both of which have been shown to modulate intestinal dysbiosis and minimize intestinal inflammation in rats. Polyphenols in herbal medicines include anthocyanins, catechinic acids, ellagic acids and gallic acids, which can be converted to biologically active metabolites by intestinal microorganisms. Therefore, the modification of the microbial community structure is beneficial to the gut.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Actis GC, Pellicano R, Fagoonee S, Ribaldone DG. History of Inflammatory Bowel Diseases. J Clin Med. 2019;8:1970. [PubMed] [DOI] Zhang YZ, Li YY. Inflammatory bowel disease: pathogenesis. World J Gastroenterol. 2014;20:91-99. [PubMed] [DOI] Plichta DR, Graham DB, Subramanian S, Xavier RJ. Therapeutic Opportunities in Inflammatory Bowel Disease: Mechanistic Dissection of Host-Microbiome Relationships. Cell. 2019;178:1041-1056. [PubMed] [DOI] Schirmer M, Garner A, Vlamakis H, Xavier RJ. Microbial genes and pathways in inflammatory bowel disease. Nat Rev Microbiol. 2019;17:497-511. [PubMed] [DOI] Yue B, Luo X, Yu Z, Mani S, Wang Z, Dou W. Inflammatory Bowel Disease: A Potential Result from the Collusion between Gut Microbiota and Mucosal Immune System. Microorganisms. 2019;7:440. [PubMed] [DOI] Bei Yue, Zhi-Lun Yu, Regulation of the intestinal microbiota: An emerging therapeutic strategy for inflammatory bowel disease, World J Gastroenterol. Aug 14, 2020; 26(30): 4378-4393, [PubMed] [DOI]