This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
While many people take probiotics to support their general digestive health, they are also used to treat certain intestinal problems such as gastroenteritis and a condition called pouchitis. But could these good bacteria also be used to treat ulcerative colitis (UC)?
1. Should I take probiotics for ulcerative colitis?
Ulcerative colitis is an inflammatory bowel disease that causes bloody diarrhea, abdominal cramps, and bloating. The disease often recurs and goes into remission, meaning that there are times when the disease is silent and other times it flares up, causing symptoms.
Standard medical treatment for ulcerative colitis has two components: Treating active flare-ups and preventing flare-ups. With traditional treatment, active flare-ups are often treated with corticosteroids such as prednisone. Flare-ups are prevented with maintenance treatment, that is, with the long-term use of certain medications.
See if probiotics can help meet either of these treatment needs.
2. Can probiotics help prevent flare-ups?
The answer to this question is probably no. A 2007 review of clinical studies on the use of probiotics for ulcerative colitis flares found that probiotics did not shorten the duration of flare-ups when added to conventional treatment. often.
However, people in studies taking probiotics reported fewer symptoms during flare-ups, and these symptoms were also less severe. In other words, while probiotics don't end flare-ups any faster, they do seem to make flare-up symptoms less frequent and less severe.
Can probiotics help prevent flare-ups?
The use of probiotics for this purpose shows more promise.
Several studies have shown that probiotics may be as effective as traditional Ulcerative Colitis medications, including the gold standard treatment mesalazine.
A 2004 German study followed a group of 327 patients with a history of Ulcerative Colitis, giving half of them mesalazine and the other half probiotics (Escherichia coli Nissle 1917). After one year of treatment, the mean duration of remission (times without flare) and quality of remission in both groups were the same.
Similar results have been seen in other studies. And another probiotic, Lactobacillus GG, may also be helpful in maintaining remission of ulcerative colitis.

3. How do probiotics help treat ulcerative colitis?
Probiotics can help treat ulcerative colitis because they address the real cause of the condition.
Ulcerative colitis is thought to be caused by problems with the immune system in the gut. Your immune system helps your body fight disease, but it can sometimes attack and target your own body in an attempt to protect it from perceived danger. When this happens, it is called an autoimmune disease.
In the case of ulcerative colitis, an imbalance of bacteria in the large intestine is thought to be a perceived danger that causes the immune system to react.
4. Can Probiotics Make Ulcerative Colitis Worse?
Probiotics can be helpful by providing good bacteria that help restore the balance of bacteria in the gut, eliminating the problem the immune system is reacting to. Once the perceived danger is gone, the immune system can calm down or stop its attack.
As we said before, probiotics can help increase the time between flare-ups and can make flare-up symptoms less severe. Additionally, probiotics can be cheaper than conventional Ulcerative Colitis drugs, and they may be safer in the long run.
Probiotics may also protect against other intestinal problems such as Clostridium difficile colitis and traveler's diarrhea.
There are many benefits, but there are some disadvantages to using probiotics with ulcerative colitis. The main thing is that they may not be helpful in making remission faster during an ulcerative colitis flare-up.
Another thing is that some people should use them with caution. Probiotics contain live bacteria, so they may increase the risk of infection in people with compromised immune systems (such as those taking high-dose or long-term corticosteroids). This is because a weakened immune system may not be able to keep the live bacteria under control and infection may result.
Advantages of probiotics for ulcerative colitis
May help prevent flare-ups of ulcerative colitis May reduce symptoms during flare-ups No serious side effects shown so far Less expensive other ulcerative colitis medicines May be safer for long-term use than other ulcerative colitis medicines May protect against other intestinal diseases, such as C. difficile infections
Continuous flare-ups during handling Caution should be exercised when given to immunocompromised individuals
5. Where can I buy probiotics?
There are countless types of probiotics available and many strains of microorganisms that can be used in them. Two of the most common bacteria used are Lactobacillus and Bifidobacterium.
You can get probiotics from a variety of sources. You can find them in foods like yogurt, kefir (a fermented drink made from cow's milk), and even sauerkraut.
You can also take them as a supplement, in forms like capsules, tablets, liquids or gum. Your local pharmacy may have several options available.
If you are thinking about taking probiotics, you should be aware that unlike prescription drugs, probiotic supplements are not regulated by the US Food and Drug Administration (FDA). ). This means that the FDA does not test whether supplements are safe or effective before they are put on the market.
If you want guidance on how to find a high-quality probiotic, talk to your doctor.
Side Effects
To date, there have been no serious side effects associated with prolonged use of probiotics for Ulcerative Colitis. In a review of studies, the incidence of side effects in people taking probiotics was similar (26% versus 24%) in those taking mesalazine.
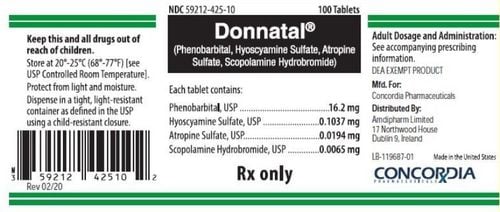
Other medications
Although taking a probiotic may help improve your Ulcerative Colitis, your doctor may also prescribe medication to help induce or maintain remission. These medications are divided into four main categories, which include:
Aminosalicylate Corticosteroid Drugs Immunostimulators Biologics Talk to your doctor
Although probiotics are easy to use and have few side effects, you should be told Talk to your doctor before adding them to your ulcerative colitis treatment plan. This is especially important if you have a compromised immune system or are being treated with high-dose corticosteroids.

And definitely do not use probiotics to replace any ulcerative colitis medication or treatment that your doctor has recommended without first confirming with your doctor.
But if you and your doctor think probiotics are the next option to consider for your ulcerative colitis treatment plan, ask your doctor for help in finding a good probiotic. best for you. You may have nothing to lose - except maybe some flare-ups of ulcerative colitis.
If you have a need for consultation and examination at Vinmec Hospitals under the national health system, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesHenker J, et al. Probiotic Escherichia coli Nissle 1917 (EcN) for successful remission maintenance of ulcerative colitis in children and adolescents: an open-label pilot study. DOI: doi.org/10.1055/s-2008-1027463 Information for consumers on using dietary supplements. (2016). fda.gov/Food/DietarySupplements/UsingDietarySupplements/default.htm Kruis W, et al. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. DOI: dx.doi.org/10.1136%2Fgut.2003.037747 Mallon P, et al. Probiotics for induction of remission in ulcerative colitis. DOI: doi.org/10.1002/14651858.CD005573.pub2