This is an automatically translated article.
Video content is professionally consulted by BSCK II Nguyen Bang Phong, Cardiology Center - Vinmec Times City International Hospital
Currently many people still do not fully understand the concept of syncope and are not prepared for this condition. In fact, fainting, also known as unconsciousness, is a condition in which a person loses consciousness for a short time due to low blood pressure that prevents blood from reaching the brain, or because the heart cannot pump enough blood. oxygen to the brain.
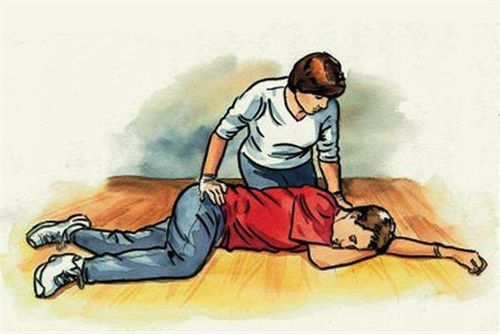
When fainting, the patient often falls to the ground when suddenly fainting, however, this is different from the seizures that cause the patient to convulse, after fainting, the patient will regain consciousness later seconds and feel normal again, in many cases feeling very tired after waking up.
According to statistics, about 95% of patients have the first signs of fainting before the age of 40 and if the first sudden fainting occurs after the age of 40, it is most likely related to some medical problem, adults With age, fainting is usually caused by cardiovascular disease, low blood pressure or as a side effect of medication.
In an upright or leaning position, blood tends to pool in the legs, which more or less makes the blood flow to the heart and then to the brain to decrease. Normally, the body responds to autonomic mediated by a slight increase in blood pressure and heart rate. If the autonomic nerve is impaired, the blood pressure not only does not increase, but also decreases, causing fainting due to a drop in blood pressure in the standing position.
If the autonomic reflex is disturbed, the heart rate not only does not increase, but on the contrary also decreases, even asystole for a short time, then fainting occurs, called syncope due to vagus. Some cases of neuro-responsive disorder are characterized by an excessive increase in heart rate, usually by 30 beats/min or more, known as orthostatic reflex tachycardia. On that basis, the cases of fainting, especially multiple syncope, were determined to be syncope not due to heart disease, the cases need to distinguish syncope or epilepsy, pseudosyncope due to psychological disorder, or multiple falls with no identifiable cause, a tilt table test (NPBN) is indicated.
The tilt table test is conducted in a quiet, temperature-stable room with an oxygen supply, suction head, blood pressure monitor and electrocardiogram, electrocardiogram recorder, emergency equipment and medications. Before performing the tilt table test, the patient should be thoroughly explained about the principle, procedure and possible response scenarios for the best coordination. Patients need to fast and drink 4 hours before the procedure to avoid choking on food or water when fainting.
When performing the tilt table test, the patient is placed supine on a table that can be raised about 60-70° and rapidly lowered to the horizontal position in 10 seconds. Secure straps at the knee, at the hip and at shoulder level. Place an intravenous line through which to administer medication if needed. The tilt table test will take place through the following phases:
Pre-test phase: Passive phase (20 minutes) Drug phase (15 minutes) Currently, the tilt table test is a fairly simple technique, easy to perform and safe , is effective in identifying syncope due to orthostatic hypotension or reflex, or distinguishing syncope from epilepsy, psychogenic pseudosyncope.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.