This is an automatically translated article.
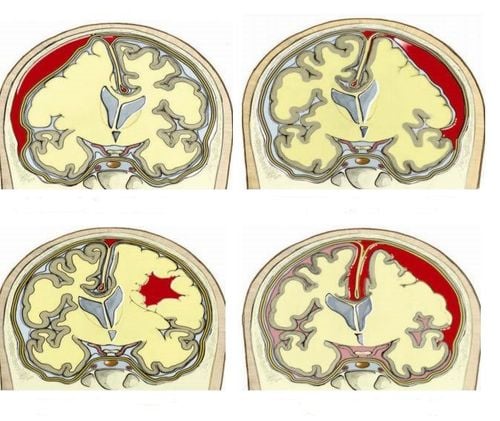
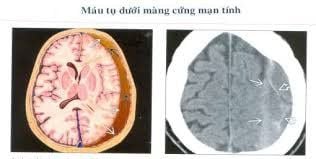
A subdural hematoma is usually caused by a traumatic brain injury that causes a blood clot to form in the subdural space, which is the space between the dura and the arachnoid. A subdural hematoma in adults can also be chronic due to weakening of the blood vessel walls, which is common in the elderly.1. What is a subdural hematoma?
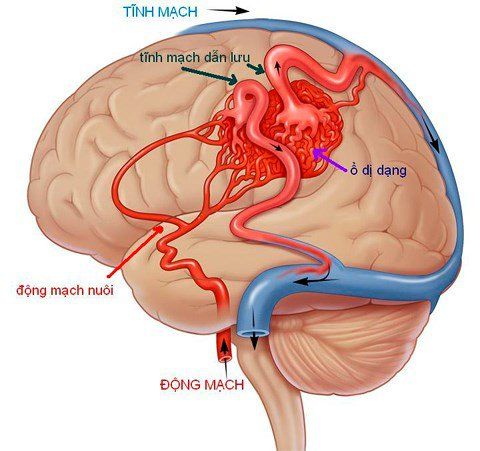
The meninges have three layers in order from the outside to the inside: the dura mater, the arachnoid, and the soft membrane. Accordingly, the brain also has three meningeal compartments respectively: the epidural space (this is the virtual space between the skull and the dura mater), the subdural space (located between the dura mater and the arachnoid) and the subarachnoid space (located between the dura mater and the arachnoid membrane). between arachnoid and soft membranes).Subdural hematoma is a condition in which a blood vessel in the subdural space ruptures causing the formation of a hematoma in the subdural space, usually after traumatic brain injury.
Subdural hematomas are classified as:
Acute subdural hematoma: a hematoma that forms rapidly either immediately or within a few hours. Subacute subdural hematoma: a hematoma that forms 3 to 14 days after trauma. Chronic subdural hematoma: hematoma that has formed more than 2-3 weeks after injury.
2. Causes of subdural hematoma
Tear of a meningeal vein or artery causes blood to flow into the space between the dura mater and the arachnoid. Causes of subdural hematoma include:Traumatic brain injury. This is the most common cause. Brain atrophy stretches blood vessels and increases the risk of bleeding even with very minor trauma. This condition is common in the elderly, alcoholics, with a history of traumatic brain injury. Reduced vascular wall strength commonly causes subdural hematomas in adults over 60 years of age. Coagulation disorders that cause spontaneous subdural bleeding such as anticoagulants (vitamin K antagonists, antiplatelet agents), hemophilia (haemophilia A, haemophilia B), thrombocytopenia. Cerebral vascular malformation, cerebral aneurysm. Hemorrhagic meningioma Complications from neurosurgery
Máu tụ dưới màng cứng ở người lớn thường xảy ra sau chấn thương sọ não
3. Symptoms of subdural hematoma
Symptoms of a subdural hematoma depend on the duration, rate of bleeding, and the size of the hematoma.Acute subdural hematoma usually presents immediately after head trauma. The patient may be comatose at the time of injury or have a gradual decline in consciousness and coma after a period of awakening. If a large hematoma compresses the brain parenchyma, there will be signs of increased intracranial pressure such as headache, vomiting, dilatation of copper, cranial nerve palsies, weakness of limbs, stiff neck, even convulsions. Subacute subdural hematoma, symptoms such as loss of consciousness, headache, nausea, and vomiting become apparent only after 3 to 14 days. Chronic subdural hematoma, symptoms usually appear about 2 to 3 weeks after head injury, sometimes months. The manifestations are silent and tend to increase gradually such as anorexia, nausea, vomiting, lethargy, headache, excessive sleep, confusion, disturbances in consciousness, visual disturbances, weakness and paralysis of the limbs on one side. Seizures can also sometimes occur. Chronic subdural hematomas are sometimes difficult to detect and can be missed, especially in the elderly.
4. Diagnosis of subdural hematoma
In addition to the clinical symptoms, the diagnosis of subdural hematoma is also based on clinical examination.Blood tests to count platelets, tests for coagulation function, quantification of clotting factors if hematologic disease is suspected. Computed tomography of the brain is the most useful and widely used imaging test in traumatic brain injury. Acute subdural hematoma presents as a crescent-shaped, hyperattenuating mass around the cerebral cortex. In contrast, subacute and chronic subdural hematomas show a crescent-shaped mass, mixed or hypodense, and deformed brain surface. Brain magnetic resonance imaging is more sensitive in detecting intracerebral hemorrhage, small subdural hematoma, and subdural hematoma in the interhemispheric cleft or tentacle of the cerebellum. Cerebral angiography is indicated when the cause of the subdural hematoma cannot be found by CT-Scan or brain MRI. Cerebral angiography can detect vascular malformations, aneurysms, and wall lesions

Máu tụ dưới màng cứng là một bệnh phức tạp
5. Treatment of subdural hematoma
Treatment of a subdural hematoma depends on the time of hematoma formation, the size of the hematoma, and the clinical symptoms.If the subdural hematoma is acute but the hematoma is small, asymptomatic, or asymptomatic, sometimes patients need only symptomatic treatment and careful monitoring. Because the body will secrete substances that dissolve blood clots. If new signs are present, the condition worsens, or the CT scan shows an enlarged hematoma, surgery may be necessary.
Surgery can be performed as soon as the subdural hematoma has formed if the hematoma is large, there are signs of brain parenchymal compression such as increased intracranial pressure or causes such as weakness in the limbs, speech disorders. Surgical methods include drilling a hole in the skull or opening the skull cap to decompress.
Skull hole drilling is the process of making a small hole on the site of a hematoma formed by drilling through the skull. Through these small holes, the hematoma can be taken or sucked out. The incision will be sutured closed or skin clamps used. Craniotomy Decompression is the process of exposing the brain and meninges by cutting off part of the skull. This method helps reduce pressure inside the skull and opens the way to remove the hematoma. The portion of the skull that was cut out is then repositioned and fixed in place. In summary, subdural hematoma in adults is a complex disease, so emergency, treatment and resuscitation need to be performed by qualified medical facilities with a team of qualified doctors. specialized training. The treatment requires comprehensiveness, perseverance to follow the patient and strictly implement the technical process to have the opportunity to minimize the patient's symptoms.
Vinmec International General Hospital is proud to be one of the hospital systems in the country that is invested in a system of modern equipment and machines with a team of doctors who are top experts who can conduct imaging, diagnosis and detection of cranial pathologies for high diagnostic and treatment efficiency.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.