This is an automatically translated article.
Subcutaneous adipose tissue is considered one of the largest endocrine organs in the body, it is also an active tissue for cellular reactions and metabolic homeostasis, rather than a motor to store energy.
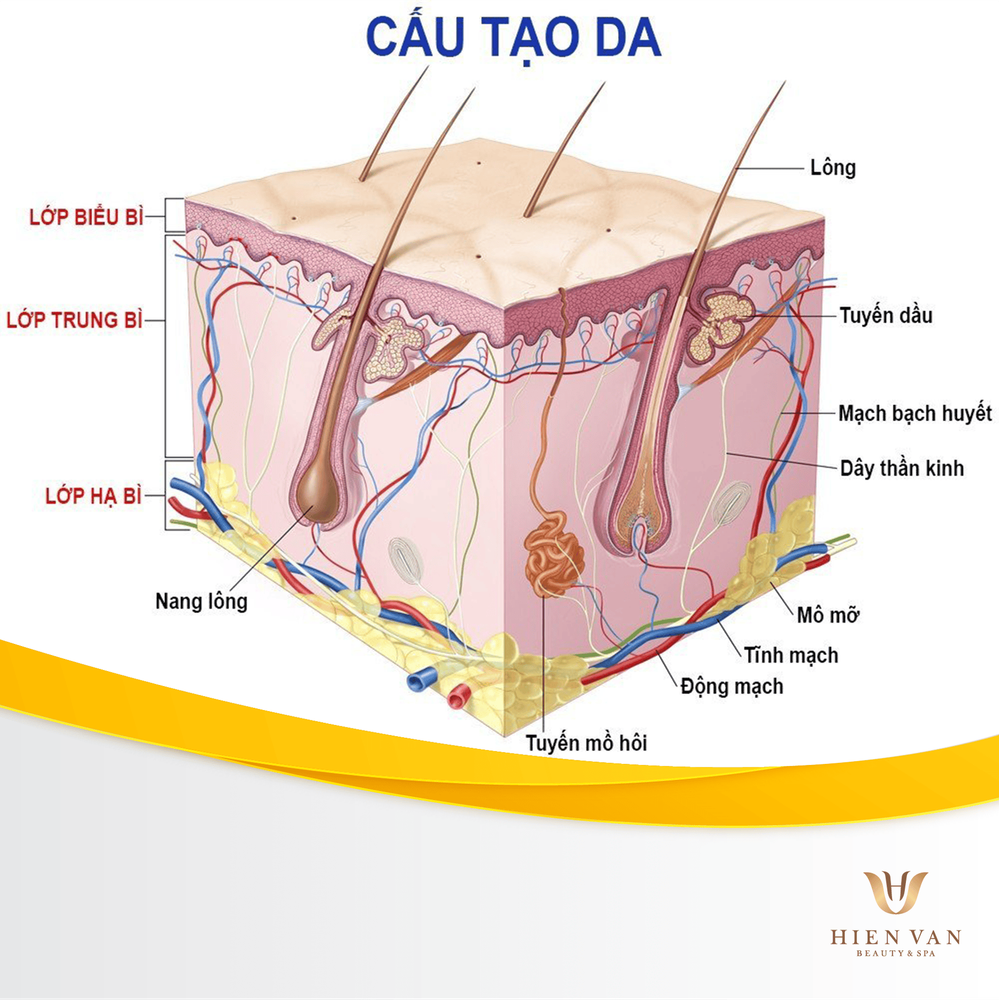
1. What is subcutaneous adipose tissue?
Adipose Tissue (AT) is considered the largest endocrine organ in the body and acts for cellular responses and metabolic homeostasis rather than as an inert tissue for energy storage. quantity. The functional pluripotency of AT relies on its ability to synthesize and release a large number of hormones, cytokines, extracellular matrix proteins, growth factors as well as vascular activity, collectively known as adipokines. They influence many physiological and pathophysiological processes.
AT dysfunction is associated with the onset of important diseases including obesity, type 2 diabetes, dyslipidemia, or nonalcoholic fatty liver disease. The underlying mechanisms of AT dysfunction include adipocyte hypertrophy and hypertrophy, AT inflammation, impaired extracellular matrix remodeling, and fibrosis along with altered secretion of adipokine. The potential role of brown AT is also seen as an excretory organ in protection against obesity.
Subcutaneous adipose tissue is classified into two types as WAT (white adipose tissue) and BAT (brown adipose tissue). These tissues have different morphology, biochemical and functional characteristics. WAT is adipose tissue that makes up at least 10% of the body weight of a normal healthy adult. It is mainly located in subcutaneous and visceral depots and can store energy in the form of triglycerides, regulating energy homeostasis through its own secretory activity. White adipocytes are spherical with variable size, the change in size depends on the size of the lipid droplet. In contrast, BAT stores lipids in polymolecular lipid droplets specifically the sympathetic nervous system (SNS) which are highly vascular and internally nourished. In addition, brown fat cells themselves have a very unique cellular and molecular structure. The thermogenic property of brown adipocytes is accomplished by their very dense, large, spherical and multilayered mitochondria.
2. Historical perspective on adipose tissue biology
The first published citation referring to adipose tissue dates back to 1837. Subsequent single AT citations appeared in the literature until the 1940s, including a 1933 publication in the Journal of Biochemistry. examined fatty acid unsaturated levels in human AT in relation to its depth from the skin surface. The earliest recognized function of adipocytes is to store energy in the form of triacylglycerols (TAGs). It was not until the mid-1980s that the secretory function of AT and the production of adipocyte-specific proteins were revealed. At that time, a serine protease called adipsin secreted from the cultured adipocytes and reported weight loss in mouse models compared with lean congeners. The acylation-stimulating protein, a member of the alternative complement family, was also revealed to be produced by AT and involved in lipid storage. Although the function of these AT secretion products is still poorly understood, the discoveries suggest that adipocytes and AT are important sources of a wide variety of protein products, including many endocrine hormones.
Arguably one of these most important discoveries was leptin, a bona-fide-derived hormone that not only acts as an afferent "adipostate" signal of fat mass to the centers of fat. brain in regulating body weight, but also have peripheral activities affecting glucose metabolism and immune function.
In addition, fat cells are also very sensitive to insulin and participate in the regulation of blood glucose levels. The action of insulin on adipocytes stimulates glucose uptake and regulates lipid metabolism by increasing accumulation and decreasing breakdown of TAGs in adipocytes.
Today, obesity and its associated epidemics have become a global problem with the majority of the world's population living in countries where overweight and obesity account for more deaths than malnutrition. Excess AT is a major challenge for chronic disease prevention and health worldwide. This global pandemic can be attributed to developing economies and the adoption of motorized transport, urbanization, commercial growth, industrialization, more sedentary lifestyles, the transition nutritional shift to processed foods and high-calorie diets over the past 30 years. Besides preventing obesity by promoting a healthy lifestyle through diet and exercise, one of the best ways for modern doctors and scientists to combat the global threat of obesity is better understanding of AT.
Mô mỡ dưới da được coi là một trong những cơ quan nội tiết lớn nhất trong cơ thể.
3. Adipose tissue metabolism and inflammation in obesity
Subcutaneous adipose tissue is a highly dynamic organ, metabolically active and involved in a multitude of physiological processes. The expansion of adipose tissue during the development of obesity is often accompanied by adipose tissue dysfunction, thereby contributing to metabolic and endocrine disturbances. Adipose tissue dysfunction characterized by adipocyte hypertrophy, impaired lipid metabolism, inflammation, disproportionate deposition of extracellular matrix components, and inadequate vascularization appear to play a prominent role in insulin resistance and systemic inflammation. Furthermore, there may be a link between adipose tissue dysfunction and lung diseases. Targeting adipose tissue dysfunction may provide a valuable strategy to improve myocardial health and lung function in obese individuals and those with myasthenia gravis, who have is the relative excess of subcutaneous adipose tissue.
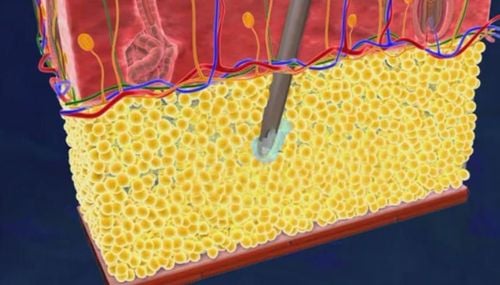
4. Isolation of stem cells derived from adipose tissue
Adipose tissue is mainly composed of adipocytes and partly vascularized (SVF), including pericytes, endothelial cells, monocytes, macrophages, and ASCs. ASCs are dissociated from the stromal vascular portion of lipoaspirates. Newly dissociated ASCs are also commonly associated with different cell types such as endothelial cells, fibroblasts, progenitor cells, mast cells, and cells from smooth muscle. After a few initial cell migrations, ASCs in the culture persisted leading to population homogeneity. To isolate ASCs, liposuction-derived adipose tissue involves shredding the adipose tissue sample, digesting with collagenase, and washing the tissue with phosphate-buffered saline followed by centrifugation to separate the stromal stromal population in the stromal layer. bottom of the tablet out of fat cells. The extraction of ASCs is being done using liposuction and studies have used these cells in.
ASC can be maintained under well-defined environmental conditions with and without serum. The cellular components in ASC isolation differ based on the influence of many factors such as age, tissue type, isolation procedure, culture and experimental conditions, number of cells dissociated as well as storage. cell. ASCs can be purified based on the expression profile of surface-labelled antigens such as bone marrow MSCs. The lack of reliable cell surface marker antigens for ASC enrichment is problematic in isolating a pure ASC population.
5. Adipose tissue - Physiology for dysfunctional metabolism
Like the obesity epidemic, our understanding of fat cells and adipose tissue is expanding. In the last decade alone, significant advances have led to new insights into the contributions of adipose tissue to normal physiology and obesity-related complications, putting adipocyte biology at the center of attention. of the global pandemic of metabolic diseases. Arguably, one of the most important discoveries of the last two decades of adipocyte research is that not only do fat cells secrete endocrine hormones, but fat cells and adipose tissue secrete a variety of effects. Various nuclei, including exosomes, miRNAs, lipids, inflammatory cytokines, and peptide hormones act at both endocrine and endocrine levels to influence local and systemic metabolic responses. The origin of adipocytes through progenitor cells and adipocyte development are discussed. Inflammation, healthy fat metabolism, and adipose tissue expansion are also considered.
Mô mỡ dưới da chủ yếu bao gồm các tế bào mỡ và một phần mạch đệm
6. Endocrine properties of subcutaneous adipose tissue
Adipocytes and other AT cells secrete a variety of mediators, including exosomes, miRNAs, lipids, inflammatory cytokines, and peptide hormones that act in both endocrine and endocrine modes. Although adipocytes secrete a wide variety of bioactive molecules with broad systemic effects that contribute to many physiological and pathological processes, the autoendocrine and endocrine activities of these molecules are very important. complex, our understanding of these processes may be sketchy. However, considerable progress has been made in the study of three endocrine hormones that are produced almost exclusively in adipocytes and have functions in the regulation of food intake, reproductive axis, insulin sensitivity, immune response Translate. These hormones are leptin, adiponectin, and resistin.
Although not directly produced in human adipocytes but secreted by AT macrophages, resistin has a similar function in mice and humans. Dysregulation of any one of these hormones may contribute to systemic metabolic dysfunction as well as to the pathogenesis of chronic metabolic diseases and certain types of cancer.
7. The promise of fat cell biology
Important considerations in the study of adipose tissue are complexity and cellular heterogeneity. AT stores may exist in close association with other organs and function physiologically as metabolic stores that store excess energy in the form of lipids in a protective manner, or they may promote dysfunction systemic metabolism by secreting excess lipids, inflammatory adipokines.
Currently, we are going through a new and exciting phase in AT research with focus shifting to the recognition of neglected AT depots, ever-expanding adipocyte types, and complex developmental origins. complex of subcutaneous adipose tissue. Adipocytes are important secretory cells that contribute a variety of circulating proteins, including endocrine hormones. Of course, adipocytes also produce lipids and can release genetic material with profound systemic functions. Much remains to be discovered about the types of nerves present in adipose tissue and how they vary depending on the type of AT and location. How these AT nerves function to regulate metabolic homeostasis is a current focus of adipocyte biology. Recent advances in whole-tissue AT imaging and studies of brain-fatty communication suggest that we are only just beginning to explore the capacity and function of the AT nerve and many questions remain. answered in this area. Studying the molecular pathways connecting intrinsic AT to insulin action in obesity and diabetes may provide insight into our understanding of the pathogenesis of transitional disease states. chemical.
Another growing area of fat cell biology is the impact of exercise on fat cell function. Recent studies have shown that subcutaneous AT transplantation from exercise-trained mice improves glucose tolerance and insulin sensitivity in recipient mice. It is particularly suggested that beneficial exercise regenerates AT to improve systemic metabolic health. The importance of AT for whole-body energy metabolism is well established. However, the effects of different types of endurance or resistance exercise on adipose tissue dynamics have not been clearly studied, particularly in the context of obesity and other metabolic disease states.
A newly discovered pathway suggests that lipids can be released by adipocytes as exosome-sized lipid-filled vesicles. This process occurs independently of canonical lipolysis pathways and adipose cell exosomes deliver excess lipids to local macrophages in obesity. Other novel endocrine regulatory pathways have also been demonstrated in AT. These paradigm-shifting observations demonstrated that extracellular vesicles (EVs) from endothelial cells in adipose tissue can deliver lipids and proteins to neighboring adipocytes. This EV communication between endothelial cells and adipocytes in AT is bidirectional and is regulated by fasting/feeding and under obesity conditions.
Although it was once considered a mere energy storage site, AT is now considered an important endocrine organ and inflammatory cell signaling site, which governs not only survival but also important role in reproduction and metabolic homeostasis. As scientific methods to study AT continue to advance rapidly, our understanding of the metabolic, biomechanical, immunological and secretory functions of AT in normal physiology and metabolic disease also.
Leading in applying many modern stem cell and gene technologies, and owning the most modern and closed tissue bank in Vietnam today, Vinmec is conducting storage and isolating stem cell cultures Tissues from different sources, in which mesenchymal stem cells from adipose tissue - which are "discarded" products after cosmetic liposuction are used in treatment and beauty.
With the above-mentioned solid foundations of people and technology, Vinmec International Hospital will soon be able to provide comprehensive and truly useful healthcare solutions that the majority of Vietnamese people are currently looking for. search.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: sciencedirect.com, ncbi.nlm.nih.gov