This is an automatically translated article.
When there are signs of brain abscess, it is necessary to take the patient to the doctor as soon as possible because the brain is an important part that controls life and all movements of the body. Brain abscess, if properly and promptly treated, will reduce the risk of death and complications later.
1. Brain Abscess
The brain is the control center of the central nervous system responsible for controlling human behavior. Some bacteria and other organisms can get past the defenses of the cranial immune system and surrounding tissues, causing infection. The pus-filled sacs in the epidural, subdural and intracerebral locations due to pus-producing bacterial infections in the brain are called brain abscesses, causing complications such as purulent meningitis, rupture of the abscess, and brain entrapment with a high rate. mortality with a very high rate. In addition, trauma to the brain for some reason also causes brain abscess.
2. Causes of brain abscess
Often, trauma to the head, face and neck is also one of the risk factors for brain abscess.
Infections near the brain such as frontal sinusitis, ethmoid sinusitis, otitis media, mastoiditis. Bacteria enter the blood and cause diseases such as lung abscess, empyema, endocarditis, liver abscess, osteomyelitis, pyelonephritis, boils. If the brain abscess is hematogenous, the abscess is usually deep in the brain, with one or more foci in different locations.
Common bacteria that cause brain abscess are intestinal bacilli, Staphylococcus aureus, non-hemolytic streptococci, anaerobic bacteria, fungi, and amoeba.
Abscesses can be epidural, subdural and intracerebral or there are cases of brain abscess where no primary source of infection can be found.
Factors that increase the risk of brain abscess such as trauma to the head, infection near the head such as: ears, nose, nose, face, diabetes or chronic diseases, congenital heart disease birth, meningitis, people who abuse drugs or have weak or weakened immune systems such as people with cancer, people with serious illnesses, people with HIV AIDS...
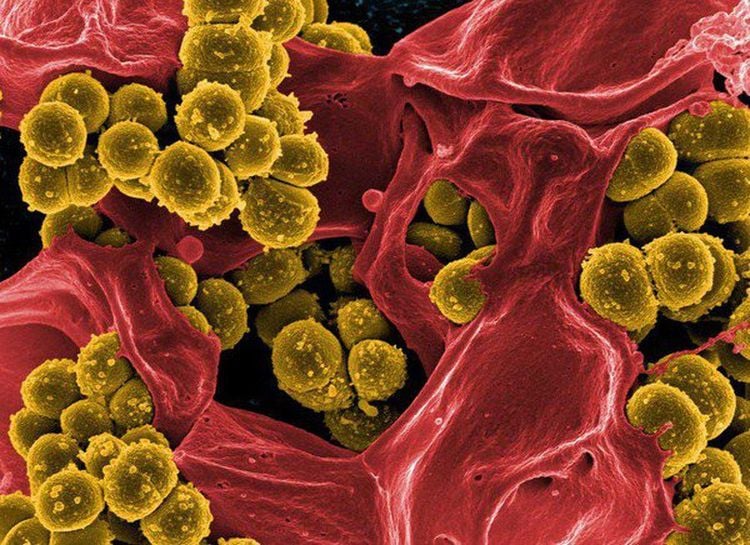
Tụ cầu khuẩn là loại vi khuẩn có thể gây áp xe não
3. The process of forming brain abscess
Brain abscess is divided into 4 stages including encephalitis stage, late encephalitis stage, early abscess rupture stage, late abscess rupture stage. Pathogenic bacteria create inflammatory foci in a place or surrounding areas according to the blood line, making the central area of pus necrotic edema strongly liquefied, the surrounding area has some fibroblasts, the outermost is the edematous area. Spread.
The necrotic area is the center of the inflammation that gradually spreads around, there are inflammatory cells such as granulocytes mixed with necrotic cells and begins to form pus. The blood vessels are transported to more to prevent the pus-filled cyst from spreading around forming a solid encirclement forming an abscess storm.
4. Diagnosis of brain abscess
Infectious syndrome lasting more than 2 to 3 weeks with fever, headache.
The syndrome of increased pressure in the brain has symptoms of headache, vomiting or altered consciousness such as agitation, lethargy, somnolence, semi-coma, coma.
Focal neurological syndromes such as central VII nerve palsy, hemiplegia are often abscesses in the cerebral hemispheres.
Aphasia due to complications from mastoiditis, temporal lobe abscess.
Ataxia, nystagmus, stiff neck causing cerebellar abscess.
The doctor ordered paraclinical tests to check the fundus, and found that about 60-70% of cases had papilledema. Blood count increased neutrophils, increased erythrocyte sedimentation rate, and increased hematocrit in patients with Fallot 4. Cerebrospinal fluid puncture should be cautious and contraindicated in the presence of papilledema, when intracranial pressure is elevated. Computed tomography can confirm the diagnosis of an abscess with a round or oval shape with clear boundaries, especially when using contrast-enhanced CT to determine the location and size of the abscess.

Chụp CT để cho kết quả chính xác nhất bệnh áp xe não
5. Treatment of brain abscess
Medical treatment using antibiotics to treat pathogenic bacteria, from 4 to 8 weeks. Cefotaxime (Claforan) 200-300mg/kg/24 hours, divided into 2 - 3 IV injections, or Ceftriaxone (Rocephine); Ceftazidime pentahydrate (Fortum) 70-100mg/kg/24h, divided into 2 - 3 IV injections. Combined with Metronidazole 40mg/kg/24h intravenous infusion divided into 2 times. Drugs to treat high blood pressure: Mannitol 20% dose 0.5g/kg x 2 times/day, from 3 to 5 days, infusion of Ringer Lactate 30-50mg/kg/day (electrolyte control). Anticonvulsants: Phenobarbital 3-5mg/kg/day in 2 divided doses or Seduxen 0.3 - 0.5mg/kg/1 time, orally. Fever reducer: Paracetamol 15mg/kg/time, orally.
Surgical treatment when antibiotic treatment is not effective, the abscess is large in size threatening to be trapped. Method of aspiration pus, isolation of bacteria and treatment according to the antibiotic chart or remove the abscess if it is large pus. After surgery, antibiotic treatment is given for 4 weeks by intravenous injection, after switching to oral for 2-4 weeks and appointment for re-examination. It took many months for the abscess to disappear on computed tomography. Patients need to be monitored after discharge as well as regular follow-up appointments under the doctor's instructions.
Brain abscess is a very serious disease and has a high mortality rate. To prevent disease, it is necessary to avoid the causes of abscesses. In addition, there must be a reasonable living diet. Limit ear, nose, throat and oral infections by taking care of your teeth regularly when you wake up and after meals. If the symptoms of sinus or tooth infection persist, the patient must be taken to a medical facility for examination and drug intervention. Especially to prevent injury accidents such as wearing helmets when participating in traffic; use labor protection equipment in occupations such as masons, carpenters, machine operators.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.