This is an automatically translated article.
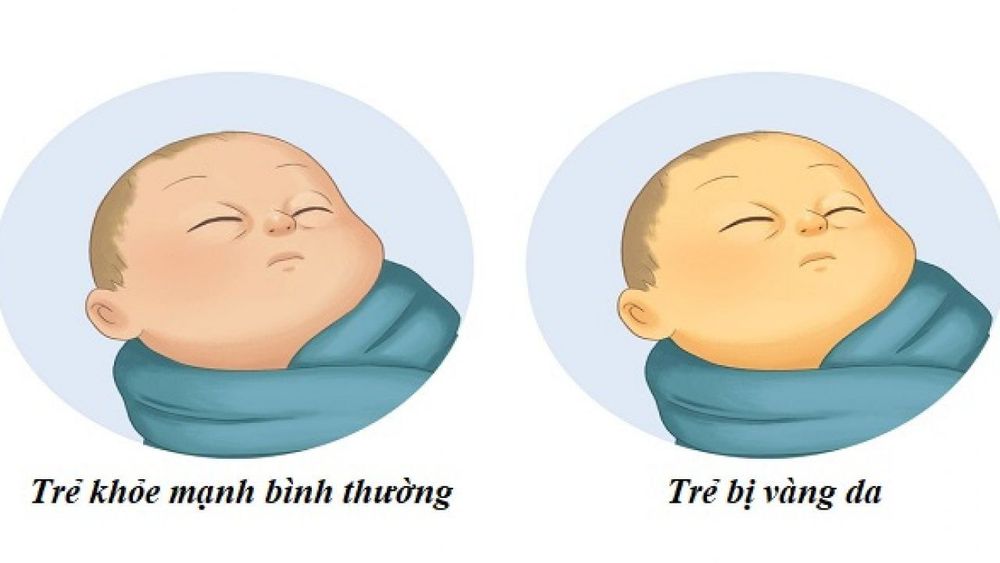
The article was professionally consulted by resident Doctor Duong Van Sy - Resident Doctor of Pediatrics - Department of Pediatrics - Neonatology - Vinmec Hai Phong International General Hospital.Jaundice is a very common condition in infants. More than half of babies are born with varying degrees of jaundice and will go away on their own. However, in some cases, persistent jaundice in infants is a sign of an underlying medical condition.
1. What is persistent neonatal jaundice?
Jaundice occurring in newborns is not a sign of liver disease. This is a fairly common physiological phenomenon. The incidence of jaundice is up to 6 out of 10 babies born at term and up to 8 out of 10 babies born prematurely.The mechanism of neonatal jaundice is explained that the newborn baby is born with a higher red blood cell count than normal. At the same time, the baby's body is constantly creating new red blood cells and breaking down old red blood cells. It is red blood cells that, when broken down, release a product called bilirubin, which is yellow in color. Therefore, the concentration of bilirubin in the newborn's body is high, so it will cause neonatal jaundice.
A few days after birth, the baby's liver will metabolize and remove bilirubin from the blood out in feces and urine. Your baby's skin will gradually fade in color. This is the mechanism of physiological jaundice in neonates and will be more common in premature infants. Whether a baby's skin is very yellow or even this color can be seen in the sclera (the white part) of a baby's eyes, most babies with jaundice are healthy and have nothing to worry about. . After that, jaundice will resolve on its own by the time the baby is 14 days old or up to 3 weeks in premature babies.
However, in a few cases, the presence of jaundice may persist for more than 2 weeks in a full-term infant and after 3 weeks in a premature infant. This will be called persistent jaundice. Although, in most newborns, long-term neonatal jaundice is usually harmless, it can still be a sign of an underlying medical condition.
Số lượng hồng cầu luôn ở mức cao gây vàng da
2. What are the symptoms of persistent neonatal jaundice?
The symptoms of neonatal jaundice commonly observed in newborns are:
The skin looks yellowish, somewhat like a tanned skin. In children of a dark-skinned race, the yellow color of neonatal jaundice can be more easily seen on the sclera of the eyes, soles of the feet, palms, and also on the sides of the mouth and tongue. The sclera (the white part around the iris) is yellowish in color. Most newborns with jaundice have only visible skin symptoms without any other symptoms, but some may also have other symptoms along with: Dark urine Pale or green stools mossy, green Lethargy, lethargy or excessive sleepiness Poor or stopped feeding.
3. What are the reasons for prolonged neonatal jaundice?
Neonatal jaundice usually manifests itself in the first few days after birth but will gradually subside with time by the time the baby is two weeks old. However, sometimes this condition can also last longer for the following reasons:
Premature babies are babies born before 38 weeks of gestation that may not metabolize bilirubin as quickly as full-term babies. Premature babies also suckle less and urinate less, resulting in a slower removal of bilirubin from the body. Babies have a condition where red blood cells break down more and more quickly than usual for other babies. This condition can happen very soon after the baby is born due to trauma during labor, birth control or even while still in the womb. Blood type incompatibility between mother and child occurs when the mother's blood type is different from that of the baby. At this time, the baby's body will receive antibodies across the placenta that cause an abnormally rapid breakdown of red blood cells. Breastfeeding but the baby is still healthy and the mother still needs to continue to breastfeed, the jaundice will fade over time. Children with congenital hematological diseases. The child has an infection. Children with thyroid dysfunction. Children have liver disease, lack of bilirubin metabolism enzymes... However, this cause is rare.
4. How is persistent neonatal jaundice diagnosed?
A doctor or even a parent can easily identify neonatal jaundice by looking at the baby's skin color in a well-lit room, preferably under natural light. In addition, the color of the sclera of the eyes, palms, feet and even the color of the child's stool and urine should also be taken into account.
Particularly for cases of persistent jaundice, the cause of this condition should be determined by supportive laboratory tests. The doctor will need to measure the true level of bilirubin in the child's blood and will decide on the course of treatment. At the same time, basic blood count, thyroid function, hepatobiliary function, and abdominal ultrasound should also be performed.

Xét nghiệm máu giúp chẩn đoán vàng da sơ sinh kéo dài
5. How long is the treatment for neonatal jaundice?
Mild neonatal jaundice will usually go away on its own within two or three weeks. For moderate or severe jaundice, the baby may need to be monitored in the hospital and actively treated to prevent dangerous complications from jaundice, although very rare.
Treatments to reduce the level of bilirubin in the blood of infants include:
Light therapy (phototherapy): The infant is placed under a special lamp that emits light in the color spectrum. blue. This light changes the shape and structure of the bilirubin molecules into a form that is easily excreted in both urine and feces. During treatment, the child is only allowed to wear a diaper and an eye patch. Holistic light therapy can be supplemented with the use of a glowing mattress. Intravenous Immune Globulin: In cases of jaundice caused by blood group differences between the mother and the baby, because maternal antibodies rapidly break down the baby's red blood cells, intravenous immunoglobulin is given intravenously. will be indicated. This is essentially a protein in the blood, which plays a role in reducing antibody levels, thereby reducing jaundice and reducing the need for blood transfusions. Transfusion: When severe jaundice does not respond to the above treatments, the neonate needs a blood transfusion. This procedure will repeatedly draw a small amount of blood from the child's body and replace the same volume with red blood cells from the donor. Consequently, it will dilute the antibodies of bilirubin from the mother, reducing hemolysis due to blood group incompatibility.

Liệu pháp ánh sáng (quang trị liệu) trị vàng da sơ sinh
Besides, if the neonatal jaundice is not severe and can be monitored at home, parents will be guided on measures to properly nourish and care for the baby during this time:
Breastfeed regularly More: This will give your baby more milk, increase bowel movements, and will increase the amount of bilirubin that is removed into your baby's stool. Breastfed babies should have eight to 12 feeds per day for the first few days of life. Formula-fed babies should have a volume of about 30 to 60 ml every two to three hours for the first week. Complementary feeding: If the baby is exclusively breastfed but the mother does not have enough milk or the baby is having difficulty feeding, the doctor will suggest giving the baby extra formula or the mother needs to express milk to supplement breastfeeding. Let children sunbathe: Early morning sunlight is not only helpful to help the jaundice subside, but also helps children absorb vitamin D well. In short, because bilirubin levels in the blood tend to increase in children's bodies. Newborns after birth, so jaundice is quite common. However, the condition should improve after 2 weeks. If after this time the child still has jaundice or is increasing gradually, the child may have underlying diseases and needs to be actively treated to reduce the bilirubin level in the blood, to avoid progression to nuclear and hereditary jaundice. severe symptoms later.
For detailed advice on neonatal jaundice as well as treatment methods, please come directly to Vinmec Health System or book online HERE.
SEE ALSO:
Jaundice in newborns Differentiating physiological and pathological neonatal jaundice How does a newborn have persistent jaundice?