This is an automatically translated article.
Articles written by MSc, BS. Khong Trong Thang, Emergency Resuscitation Department, Vinmec Central Park International General Hospital
Pericardial aspiration is used in the case of patients with pericardial effusion, which affects heart function. This technique will help aspirate pericardial fluid so that the heart can resume functioning, avoiding continued accumulation of fluid in the pericardial capsule.
1. Aspiration of pericardial fluid
Pericardial aspiration is a technique performed to drain fluid that accumulates in the pericardium. Usually people use fine needles, small catheters to aspirate and drain the fluid.
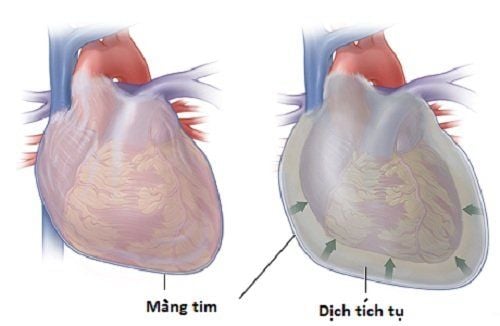
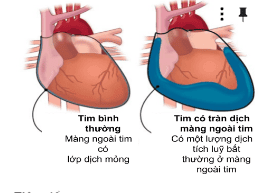
Normally, the pericardium is made up of fibrous sheaths that surround the heart, forming the pericardium with two layers. Between these two layers, there is a little lubricating fluid that helps the two layers of the pericardium reduce friction and can slide over each other when the heart contracts. In the case of pathology, there will be a lot of fluid accumulation between the two layers of the pericardium. This condition is called a pericardial effusion. When the amount of fluid is too much, it can affect the function of the heart, causing shortness of breath and shock for the patient. At that time, it is necessary to perform pericardial aspiration so that the heart can recover and avoid further accumulation of fluid in the pericardial capsule.
Tim có tràn dịch màng ngoài tim khiến người bệnh khó thở
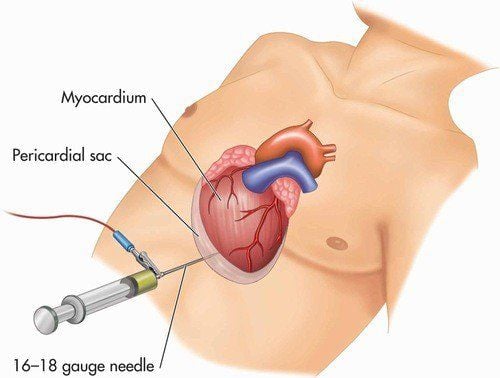
When performing pericardial aspiration technique, the doctor will use a needle to go through the chest wall into the pericardial cavity. Once the needle has entered the pericardium, a catheter (also called a catheter) will be inserted into the pericardium to drain the accumulated fluid. Immediately after drainage is complete, the catheter can be removed or kept in place to drain the fluid and prevent re-establishment.
2. Designation
Pericardial effusion can have many different causes. In which there are a number of medical diseases that cause pericardial effusion, which surrounds the heart, causing shortness of breath and chest pain. These cases, if the effusion is small, chronic (the effusion occurs gradually) can be treated medically. However, there are also cases of acute pericardial effusion, the amount of which is life-threatening and requires immediate drainage.
Pericardial puncture is performed for 2 purposes: (1) diagnosis, eg: to diagnose the cause of pericardial effusion; (2) treatment, for example, in cases of acute pericardial effusion, which will cause acute cardiac tamponade, causing shock. At that time, pericardial aspiration is indicated as an emergency to decompress to help return the heart to a favorable state of normal operation.
3. Common causes of pericardial effusion
Pericarditis , bacterial pericarditis, tuberculosis; Cancer; Pericarditis after myocardial infarction; Trauma to the heart causing pericardial hemothorax; Have autoimmune diseases; Due to radiation therapy; Due to metabolic causes such as chronic kidney failure, uremia syndrome. Pericardial aspiration is not the only means of removing fluid that surrounds the pericardium. One can also use surgery to open a window in the pericardium and drain to remove fluid. However, aspiration pericardial drainage is preferred because it is less invasive.
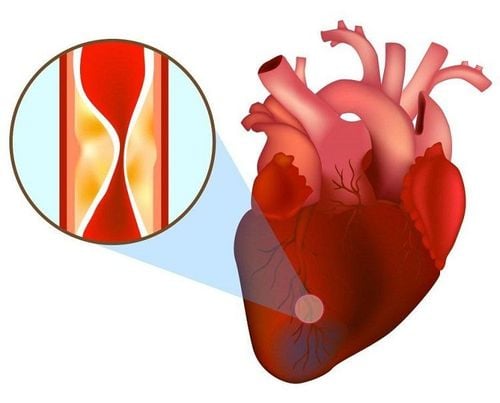
Nhồi máu cơ tim là một nguyên nhân gây tràn dịch màng tim
4. Pericardial aspiration technique
There are 3 ways to perform the pericardial aspiration technique:
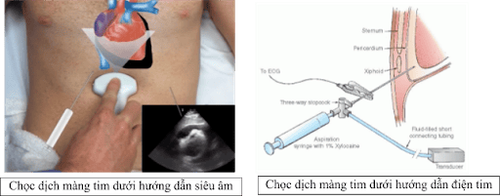
Ultrasound-guided pericardiocentesis: this is the recommended procedure, as it allows direct visualization of the needle tip as it enters the classroom pericardial effusion and it also helps the aspirator decide on the best approach for successful pericardiocentesis. Regardless of the location of the fluid on ultrasound, the nasosternal or apical approach requires emergency preparation such as cardiopulmonary resuscitation. Pericardial aspiration to monitor ECG changes: If a bedside ultrasound machine is not available, the alternative should be to use an electrocardiogram to monitor when the needle is touching the myocardium. Blind pericardial aspiration method: can be applied without the above 2 measures, but blind puncture is often associated with high mortality rate, disease progression is more severe than the previous 2 methods.
Các cách thực hiện kỹ thuật chọc hút dịch màng ngoài tim
Position of pericardial aspiration:
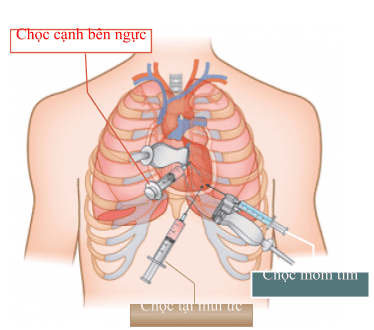
Left nasopharynx: Emergency pericardial aspiration approach from nasopharynx to the left of the costal arch is commonly used. Often a needle with an iron barrel is used to avoid tissue fragments that could block the needle. In case there is no iron-barreled needle, a metal needle with a plastic outer sheath can be used to aspirate, the needle is usually 16-18 G. If a needle without a core in the middle is used, another small technique should be applied: using a scalpel. Make an incision in the skin before inserting the needle through the skin. Once the needle has penetrated the skin, pull out the barrel and attach the needle to the fork and 20ml syringe. Push the needle towards the left shoulder, sucking while walking.
Vị trí chọc hút dịch màng tim
Using time-guided ultrasound technique, insert the needle into the most concentrated area of the pericardium. Aspirate pericardial fluid with a syringe. Withdrawal can sometimes be enough to produce an extraordinary improvement in cardiac output and blood pressure. Once the needle is in the correct position, it is easy to withdraw the fluid, drain all the fluid with the syringe attached to the fork 3. Continue to withdraw until the patient's vital signs return to normal and there is no more fluid in the pericardium. If only a small amount of fluid can be removed to stabilize the patient, there may be no need for continuous drainage. Parasternal access is another approach in the emergency pericardial aspiration procedure. Insert the needle perpendicular to the chest wall in the V intercostal space just lateral to the sternum. Use ultrasound to locate the largest outbreak and closest to the chest wall and guide the needle into the outbreak. Apical puncture: Another technique is to use ultrasound-guided apical puncture. Use a sterile needle to poke the intercostal space 1cm below and outside the apex of the heart, directing the needle to the right shoulder. Blind pericardiocentesis can be performed with a percutaneous needle puncture just below the sternum and ribs. The needle makes a 45 degree angle with the skin and pushes the needle toward the left shoulder. “Blind” pericardiocentesis is associated with a greater risk of complications than ultrasound-guided puncture. Therefore, this method should only be used in emergencies.
5. Complications of pericardiocentesis
All procedures carry risks. Risks of pericardiocentesis include:
Heart puncture, requiring surgical suturing, repair; Poke the liver; Heavy bleeding, causing acute cardiac tamponade, affecting the normal function of the heart; Pneumothorax in the chest cavity; Infection; Arrhythmia (rare but can be fatal); Heart failure and fluid in the lungs (pulmonary edema). It is also possible that after pericardial aspiration, fluid re-establishes around the heart rapidly. If this occurs, surgical removal of part or all of the pericardium is required.

Người bệnh có thể bị biến chứng suy tim, nhưng hiếm gặp
6. How to prepare for pericardiocentesis?
Patients need to fast for at least 6 hours before the procedure. The doctor will tell the patient to stop some medications before the procedure, for example, to stop anticoagulants, antiplatelets.
The doctor will ask the patient to perform some preoperative tests. These tests may include:
chest X-ray ; Electrocardiogram to check heart rate; Blood tests; Echocardiography to evaluate the amount of fluid surrounding the heart and heart function.
7. What to do after pericardiocentesis?
Often the patient will have to consult his or her doctor for specific instructions for each case. However, in general, after pericardiocentesis can:
The patient may be a little dizzy, stagger; The patient's vital signs will be closely monitored such as: heart rate, blood pressure, breathing rate, blood oxygen; If the catheter is left in place to continue draining, the doctors will monitor the catheter to keep it from becoming blocked until it is safe to remove it; The doctor will have to repeat the echocardiogram to see if the fluid has returned to effusion. Depending on the patient's condition, after a pericardiocentesis may have to stay in the hospital for a day or longer. Pericardial aspiration procedure is a very intensive technique and carries many risks of potentially life-threatening complications when performed. However, in the most necessary cases such as when the patient has pericardial effusion with signs of heart block, heart collapse then to save the patient's life, doctors will perform an emergency pericardial aspiration procedure.
To protect cardiovascular health in general and detect early signs of cardiovascular disease, customers can sign up for Cardiovascular Screening Package - Basic Cardiovascular Examination of Vinmec International General Hospital. The examination package helps to detect cardiovascular problems at the earliest through tests and modern imaging methods. The package is for all ages, genders and is especially essential for people with risk factors for cardiovascular disease.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.