This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
In recent years, two new narrow band imaging (NBI) classifications have been proposed: the NBI International Colonoscopy Classification (NICE) and the Japan NBI Expert Group (JNET) Classification. Most of the validation studies of the two new NBI classifications have been conducted within taxa by experienced endoscopists, and their use in centers varies between endoscopists with different techniques. Different endoscopic capabilities are still unknown.
1. How did the experts conduct the assessment?
In a study conducted in Asia, six endoscopists with varying degrees of experience participated in a study, the aim of which was to evaluate the clinical application and possible problems of the NICE and JNET classifications for the differential diagnosis of colorectal cancer and precancerous lesions. 87 consecutive patients with a total of 125 lesions were imaged in conventional white light colonoscopy without magnification, unmagnified NBI, and magnified NBI. The three groups of endoscopic images of each lesion were evaluated by six endoscopists in random order using separate NICE and JENT classifications. The authors then calculated the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of six endoscopists for each of the two classifications. The results of the study indicated that the sensitivity, specificity and accuracy of the JNET class 1 and 3 were similar to those of the NICE class 1 and 3 in both the highly experienced endoscopy (HEE) and less experienced endoscopist (LEE). The specificity of the JNET class 1 and 3 and the NICE class 3 classifier in both the highly experienced and less experienced endoscopists groups was >95%, and the overall agreement among Servers are good in both groups. The sensitivity of NICE classification type 3 lesions for the diagnosis of SM-d carcinoma was significantly higher in the highly experienced endoscopic group than in the less experienced endoscopic group (91.7). % vs. 83.3%; P = 0.042). Sensitivity of JNET class 2B lesions for the diagnosis of high-grade dysplasia or invasive submucosal surface carcinoma in a group of highly experienced and less experienced endoscopists are 53.8% and 51.3%, respectively. Compared with other JNET classifiers, the diagnostic ability of type 2B is the weakest. The authors concluded: The treatment strategy of the two classifications of lesions type 1 and 3 can be based on endoscopic findings. Type 2B JNET lesions require further investigation.
2. Prevalence and prognosis of colorectal cancer
What is colorectal cancer? (CRC) It is the third most common malignancy and the second leading cause of cancer death globally in 2018. The incidence and mortality from colorectal cancer is still increasing rapidly in many low- and middle-income countries. The outcome and prognosis of patients with colorectal cancer are closely related to the stage of the disease. Miller et al. reported that the 5- and 10-year relative survival rates in colorectal cancer patients were 65% and 58%, respectively, but the 5-year relative survival rates were 90% in colorectal cancer. rectum was detected at the localized stage. Therefore, it is important to improve detection rates of early colorectal cancer and precancerous lesions.
3. The role of colonoscopy in detecting precancerous lesions
Colonoscopy can directly observe intestinal lesions, so it is not a substitute for checking intestinal pathology, especially colorectal cancer. In order to improve the detection rate of early colorectal cancer and precancerous lesions, many new supportive techniques have been used in clinical practice such as appendoscopy, magnifying endoscopy, and colonoscopy. fluoroscopy, confocal laser endoscopy and electronic staining endoscopy. However, the complex and time-consuming pigment endoscopic procedure, expensive confocal laser and fluoroscopy, and these disadvantages limit the application of these new techniques.4. Electronic staining endoscope - a new step in gastrointestinal endoscopy
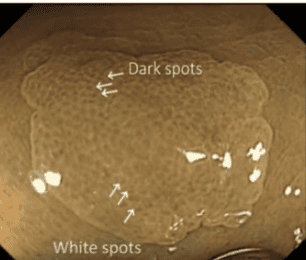
Compared with these new techniques, electronic staining endoscopy is more convenient and practical, the sensitivity and specificity in differentiating colorectal neoplastic lesions from noncancerous lesions is about 90% and 85%. Electronic staining endoscopy includes narrow-band imaging (NBI), color-enhanced bend-spectrum imaging, and i-scan, of which NBI is the most widely used. Since the appearance of NBI in 1999, it has been a reliable tool for improving diagnostic accuracy, such as distinguishing cancer from noncancerous lesions and characterizing of colorectal cancer. Through analysis of capillary vessel structure, surface structure and lesion color under NBI, researchers have proposed many classification ways to accurately assess the nature of lesions and select treatment strategies. Fit. In recent years, colorectal NBI exaggerated classifications such as the Hiroshima, Sano, Showa, and Jikei classifications have been widely used in clinical practice and played an important clinical role. However, magnifying endoscopy has not yet been widely adopted outside of Japan.
5. International classification of polypoid lesions in the colon
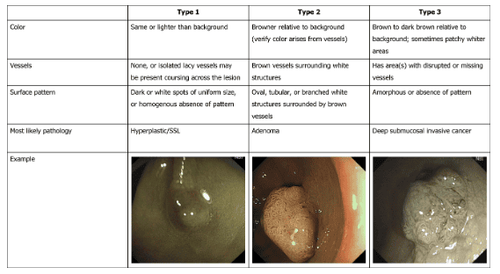
The NBI Group of Interest in Colon Tumors introduced a new NBI classification called the NBI International Colonoscopy Classification (NICE) in 2009, and studies confirming this new NBI classification have was carried out in 2012. This is the first NBI classification that can be used for both unmagnified and magnified NBI endoscopy. The NICE classification has high diagnostic accuracy in detecting non-cancerous lesions that require resection and deep submucosal invasive carcinoma (SM-d) requiring surgical treatment. However, it is difficult to distinguish high-grade dysplasia (HGD) or submucosal superficial invasive carcinoma (SM-s) from low-grade dysplasia (low grade dysplasia using the NICE classification). To address this issue, the Japan NBI Expert Group (JNET) consisting of Japanese colonoscopy specialists was organized in 2011, and a new NBI colorectal exaggerated classification, the JNET classification, was organized. published in 2014.
To the best of the authors' knowledge, most of the validation studies on the two new NBI classifications have been conducted in primary centers by experienced endoscopists, but the application in different centers among endoscopic surgeons with different endoscopic skills is unknown.For external validity, in their study, the authors evaluated the application. The clinical and probable issues of the NICE and JNET classifications in the hospital by the authors and six endoscopists with varying levels of experience participated in this study.
6. The role of polypectomy in reducing the risk of colorectal cancer
Colorectal adenoma is a precancerous lesion of colorectal cancer and resection can reduce the incidence and mortality of colorectal cancer. Therefore, in western countries, resection of all adenomatous polyps has been standardized. In clinical practice, the pathological diagnosis of all resected polyps is performed routinely and the final pathological results determine the endoscopic follow-up intervention. However, removal of all polyps and conventional pathology not only increase the risks associated with polypectomy, but also the cost of the surgery and the pathological diagnosis. Therefore, a policy of no intervention or exclusion has been proposed. The policy states that hyperplastic lesions do not require treatment and that treating these lesions may increase the adverse effects of polypectomy and the cost of medical care. As reported previously, the simple and practical NICE classification in identifying hyperplastic lesions should be left alone. In the authors' study, the sensitivity, specificity, and accuracy of the lesion were observed type 1 NICE classification for diagnosing hyperplastic lesions s and SSL in both highly experienced and less experienced endoscopic groups was >80%, with specificity and accuracy >90 %, there was no significant difference between the two groups of groups. This result suggests that endoscopists can choose a treatment plan based on the NICE classification, which can improve resection and better removal strategies.7. Classification of polyps has the ability to evaluate the carcinogenicity of colon polyps
The highly experienced endoscopic group still had high specificity and accuracy >95% when using NICE type 3 for the diagnosis of SM-d carcinoma, and the sensitivity was 91.7%, but in the group of less experienced endoscopists, the sensitivity was only 83.3%. The P value of susceptibility between the two groups was 0.042 by the Mann-Whitney U test, and the difference between the two groups for diagnosis of SM-d cancer was significant. Hayashi et al found that the sensitivity of NICE type 3 in the diagnosis of SM-d carcinoma was 94.9%. Compared with the above study, the sensitivity of the less experienced endoscopic group in diagnosing SM-d carcinoma is still low. This result may be related to the lack of experience in diagnosing SM-d carcinoma in the less experienced endoscopic group. Therefore, endoscopists in the less experienced group of endoscopists should receive additional training to avoid missed diagnoses of SM-d carcinoma.
8. The role of JNET with high magnification
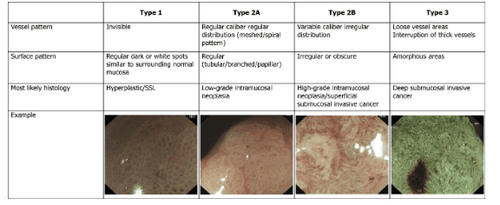
To obtain an accurate histological diagnosis, high-grade dysplastic carcinoma or SM-s should be resected by whole- or surgical EMR/ESD rather than partial EMR (pEMR). However, in clinical practice, the authors were unable to define an endoscopic treatment strategy, such as pEMR, monolithic EMR/ESD, or surgery, because NICE type 2 is difficult to differentiate from dysplastic carcinoma high-grade or SM-s with low-grade dysplasia. To solve this problem and unify the current NBI classifiers, the JNET classifier with magnification was proposed. The principles and characteristics of the JNET classification are as follows: Imagination is primary and the basis is the NICE classification, NICE type 2 is divided into subtypes 2A and 2B using exaggerated results, because Magnifications do not require color estimation, classification does not include color detection, and basic findings include surface patterns.
9. Polyps are diagnosed with early cancer on endoscopic electronic staining
The authors' results show that the sensitivity, specificity, and accuracy of JNET classifiers 1 and 3 are similar to NICE classifiers 1 and 3 in both the highly experienced and and the specificity of the JNET class 1 and 3 and NICE class 3 classifications in both the highly experienced and less experienced endoscopic groups were >95%. Sensitivity, specificity, accuracy, PPV and NPV of JNET class 2A lesions for the diagnosis of low grade dysplasia in the highly experienced endoscopic group were 82.5%, 90, respectively. .0%, 81.9%, 93.3% and 58.5% and 82.5%, 91.1%. 84.5%, 96.7% and 62.1% respectively in the group of less experienced endoscopists. The results are similar to those of Sumimoto et al.
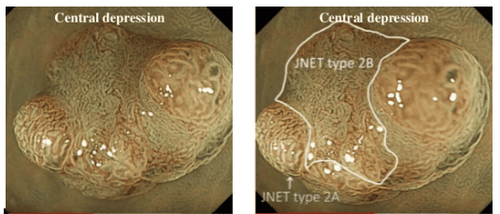
NICE types 1 and 3 and JNET types 1, 2A and 3 lesions show excellent diagnostic capacity in both the highly experienced and less experienced endoscopic groups. When confidence is high, the treatment strategy of NICE types 1 and 3 and JNET types 1, 2A, and 3 lesions can be determined based on the results of the endoscopic examination. Type 2B JNET lesions require further examination, such as magnifying endoscopy or endoscopic ultrasonography, to accurately assess the depth of invasion to select an appropriate treatment strategy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.