This is an automatically translated article.
Article written by Master, Doctor Ha Thi Thu Hien - Pathologist - Laboratory Department - Vinmec Times City International Hospital
Cervical cancer is a dangerous disease, with the incidence and mortality rate ranked second among genital cancers in women today. So what is cervical cancer? Why is this disease so dangerous and has a high mortality rate?
1. Risk factors for cervical cancer
A risk factor includes anything that increases your chances of getting the disease. Different types of cancer have different risk factors. For example, exposing the skin to sunlight with a lot of ultraviolet rays is a risk factor for skin cancer. Smoking is a risk factor for many cancers. But having one, or even several, risk factors, doesn't mean you'll get the disease.
Certain risk factors can increase your chances of developing cervical cancer. Women without any of these risk factors rarely get cervical cancer. Although these risk factors may increase the odds of developing cervical cancer, many women with these risks do not develop cancer.
When thinking about risk factors, focus should be on those that can be changed or avoided (such as smoking or HPV infection), rather than those that cannot be changed (such as age). and family history). However, it is still important to know about the risk factors that cannot be changed, as women with these factors should have regular screening tests to detect cervical cancer early.

2. Modifiable risk factors
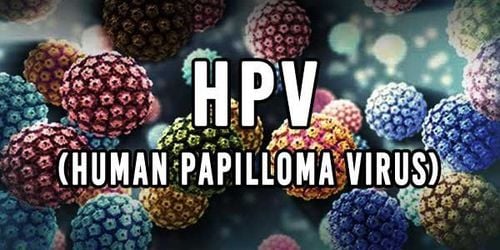
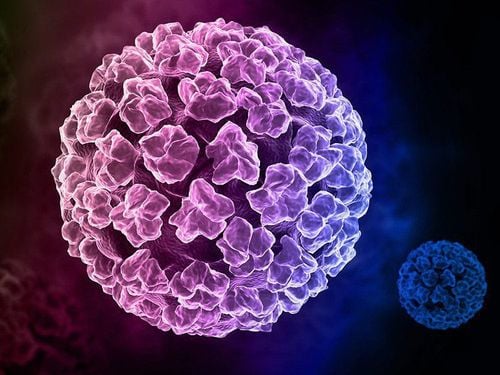
Human papillomavirus (HPV) infection
Human papillomavirus (HPV) infection is the most important risk factor for cervical cancer. HPV is a group of more than 150 related viruses. Some types cause papillomas, commonly known as warts.
HPV can infect cells on the surface of the skin and cells that line the surfaces of the genitals, anus, mouth, and throat, but does not infect the bloodstream or internal organs such as the heart or lungs . HPV can be passed from person to person through skin-to-skin contact. One way HPV is spread is through sexual activity, including vaginal, anal, and even oral sex. Different types of HPV cause warts on different parts of the body. Some cause common warts on the hands and feet; Others tend to cause warts on the lips or tongue. Certain types of HPV can cause warts on or around the female and male genitalia and in the anal area. These are called low-risk types of HPV because they are rarely associated with cancer.
Other types of HPV are considered high-risk because they are strongly associated with cancers, including cervical, vulvar and vaginal cancers in women, penile cancer in men and anal, oral, and throat cancers in both men and women.
HPV infections are common and in most people, and go away on their own. However, sometimes some people do not go away on their own and become chronic. Chronic viral infections, especially when caused by certain types of high-risk HPV, can eventually cause certain cancers such as cervical cancer.
Although there is currently no cure for HPV infection, there are ways to treat warts and the abnormal cell growth that HPV causes. In addition, the HPV vaccine is available to help prevent infection by some types of HPV and some cancers associated with these types.
Sexual history
Certain factors related to your sexual history can increase your risk of cervical cancer. The risk is most likely influenced by increased exposure to HPV.
Being sexually active at a young age (especially under 18) Having multiple sex partners Having one sexual partner is considered high risk (people who have HPV or have multiple sex partners)

Smoking
When a person smokes, they and those around them are exposed to many cancer-causing chemicals that affect organs other than the lungs. These toxic substances are absorbed through the lungs and carried into the bloodstream throughout the body.
Women who smoke are twice as likely to develop cervical cancer as women who don't smoke. Tobacco by-products have been found in the cervical mucus of women who smoke. Researchers believe these substances damage the DNA of cervical cells and may contribute to the development of cervical cancer. Smoking also makes the immune system less effective at fighting HPV.
Weakened immune system
People with HIV , the virus that causes AIDS, weakens the immune system and puts people at higher risk of HPV infection.
The immune system is important in killing cancer cells and slowing their growth and spread. In HIV-infected women, cervical pre-cancers can develop into invasive cancers more quickly than usual.
Another group of women at risk for cervical cancer are those taking drugs that suppress the immune system, such as those being treated for an autoimmune disease or those who have received an organ transplant.
Chlamydia infection
Chlamydia is a relatively common bacteria that can infect the reproductive system. It is spread through sexual contact. Women infected with chlamydia often have no symptoms and may not know they are infected unless they are tested during a pelvic exam. Chlamydia infection can cause pelvic inflammatory disease, leading to infertility.
Some studies show that women with past and current Chlamydia infections have a higher risk of cervical cancer than those who do not. Some research suggests that Chlamydia bacteria can help HPV grow and live in the cervix, which may increase the risk of cervical cancer.
Long-term use of oral contraceptives
There is evidence that long-term use of oral contraceptives increases the risk of cervical cancer. Research shows that the risk of cervical cancer increases the longer a woman takes the Pill, but the risk goes back down after stopping the Pill and back to normal many years after stopping the Pill.
Women with multiple pregnancies (> 3 pregnancies)
Women who get pregnant at a young age < 20 years old
Economic status
Many low-income women do not have easy access to adequate health care services enough, including screening for cervical cancer with a Pap test and an HPV test. This means they may not be screened or treated for cervical precancer.
Diets low in fruits and vegetables
Women whose diets do not have enough fruits and vegetables may have an increased risk of cervical cancer.
3. Unmodifiable risk factors
Diethylstilbestrol (DES)
DES is a hormone medicine that was given to some women between 1938 and 1971 to prevent miscarriage. Women whose mothers took DES (during pregnancy) are more likely to have clear cell adenocarcinoma of the vagina or cervix These cancers are extremely rare in women who have not been exposed to DES. About 1 in 1,000 women whose mothers took DES during pregnancy had clear cell carcinoma of the vagina or cervix. This means that about 99.9% of "DES daughters" do not develop these cancers.
Have a family history of cervical cancer
If you have a mother or sister with cervical cancer in your family, your chances of getting the disease are higher than if there is no family history.
4. Factors that can reduce the risk of cervical cancer
Use of an IUD
Some studies show that women who have used an IUD have a lower risk of cervical cancer. The risk effect was seen even in women who had the IUD inserted for less than one year, and the protective effect remained after the IUD was removed.
The risks and benefits of an IUD should be discussed with your doctor prior to insertion. In addition, a woman with multiple sexual partners should use condoms to reduce her risk of STIs no matter what other method of contraception she uses.

5. What causes cervical cancer?
The growth of normal human cells mostly depends on the information contained in the cell's DNA. DNA is the chemical in cells that makes up our genes, which helps control how cells work.
Certain genes control when cells grow, divide, and die: ·
Genes that help cells grow, divide, and survive are called oncogenes. Genes that help control cell growth or cause cells to die at the right time are called tumor suppressor genes. Cancer can be caused by DNA mutations that wake up oncogenes or turn off tumor suppressor genes.
Human papillomavirus (HPV) has two proteins called E6 and E7 that turn off certain tumor suppressor genes, such as p53 and Rb. This can allow the cells of the cervix to overgrow and cause changes in additional genes, which in some cases can lead to cancer.
But HPV is not the only cause of cervical cancer. Most women with HPV do not develop cervical cancer, and other risk factors, such as smoking and HIV infection, influence women exposed to HPV to be more likely to develop cervical cancer.
6. Can cervical cancer be prevented?
The two most important things you can do to prevent cervical cancer are getting the HPV vaccine if you qualify, and getting regular check-ups (health checkups) as recommended.
Most cervical cancers start with precancerous changes and there are ways to prevent this from developing. The first is to detect and treat pre-cancers before they become invasive cancers, and the second is to prevent pre-cancers.
Find pre-cervical cancer
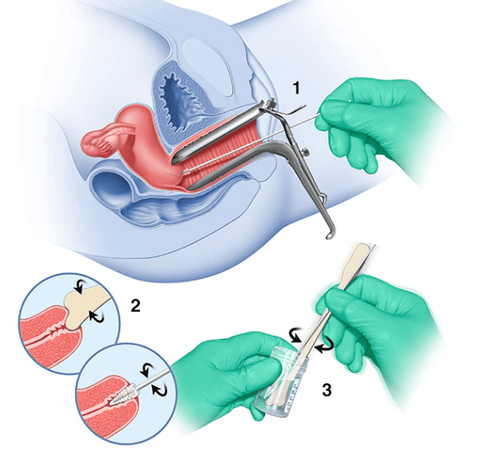
Cervical cancer screening is a proven best way to prevent cervical cancer. Traditional Pap tests (Pap smears) or liquid-based cytology and human papilloma virus (HPV) tests are specific tests used during cervical cancer screening. If a precancerous condition is detected, it can be treated, avoiding turning into invasive cervical cancer.
HPV tests reveal high-risk HPV types that are more likely to cause pre-cancers and cervical cancer.

The Pap test or cervical smear is a method used to collect cells from the cervix to be scrutinized in a laboratory for cancer and pre-cancer. Most invasive cervical cancers are found in women who do not have regular Pap tests. A Pap test can be done during a pelvic exam, but not all pelvic exams include a Pap test.
Things to do to prevent pre-cancers and cancers
Based on your age, overall health, and individual risk for cervical cancer, there are several things that can be done to prevent pre-cancers cancer and precancerous conditions.
Get the HPV vaccine
Vaccines are available that can help protect children and young adults against some HPV infections. These vaccines protect against infection with the types of HPV commonly associated with cancer, as well as certain types that can cause anal and genital warts.
These vaccines only work to prevent HPV infection - but not to treat a previous HPV infection. That's why, to be most effective, the HPV vaccine is recommended before a person is exposed to HPV (such as through sexual activity).
These vaccines help prevent pre-cancer and cervical cancer. Some HPV vaccines are also approved to help prevent other types of cancer and anal and genital warts.
American Cancer Society (ASC) recommendations:
HPV vaccination for children 9 to 12 years old. Children and young adults aged 13 to 26 years who have not been immunized or have not had the full dose, should be vaccinated as soon as possible. Immunizing youth will not prevent as effectively as vaccinating children and adolescents. The ACS does not recommend HPV vaccination for people over the age of 26. It's important to know that no vaccine can completely prevent all types of cancer-causing HPV, so routine cervical cancer screening is still needed.
Limiting exposure to HPV
HPV is passed from person to person through direct skin-to-skin contact with infected areas of the body. Although HPV can be spread by skin-to-skin contact - including vaginal, anal, and oral sex - it is not only spread during sexual intercourse. This means the virus can be spread without sex. It can even be spread from hands to genitals.
Also, HPV infection seems to be able to spread from one part of the body to another. This means the infection can start in the cervix and then spread to the vagina and vulva.
Limiting the number of sexual partners and avoiding sex with people who have had many other sexual partners can reduce the risk of exposure to HPV. A person can have HPV for many years and still have no symptoms. So it's possible that someone has the HPV virus and infects others without knowing it.
Use condoms
Condoms are some protection against HPV but they do not completely prevent infection. Because condoms cannot cover every potential HPV-infected area of the body, such as the skin of the genital or anal areas. However, using a condom during sex protects against HPV infection and also helps protect against HIV and some other STIs.
No smoking
In order to improve the quality of diagnosis and treatment, Vinmec International General Hospital has applied the ThinPrep Pap Test for early detection of cervical cancer, this new method is currently being used universally. in the US and Europe. ThinPrep Pap Test has made a breakthrough compared to the traditional Pap smear method, through membrane controlled cell transfer technology, which increases the sensitivity and specificity in detecting precancerous cells. , especially glandular epithelial cells, a type of cancer cell that is difficult to detect.
At Vinmec, the application of modern methods and procedures to ensure sterility helps to achieve the most accurate results. Screening results are delivered to your home with specific advice and recommendations for the patient
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.