This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Gastroparesis is a disease caused by delayed gastric emptying (GE), affecting about 10 million people in the United States. Diabetic and postoperative gastroparesis are common physical disorders, but the majority of patients with gastroparesis have no identifiable etiology and are considered idiopathic.
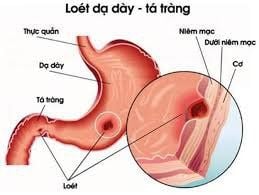
1. What is gastroparesis?
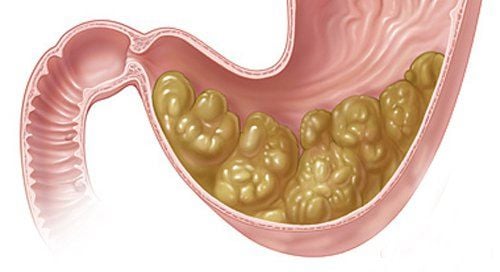
Gastroparesis (GP) is a delayed gastric emptying disease in which mechanical obstruction of the upper gastrointestinal tract has been ruled out. Typically, gastric emptying disorder is accompanied by postprandial nausea, vomiting, early satiety, bloating, and abdominal pain. Estimated to occur in 10 million (3%) people in the United States, gastroparesis can be classified as diabetic (diabetic gastropathy), postoperative (PSG), and idiopathic (IG). .
Idiopathic gastroparesis accounts for 50-60% of cases and mainly affects females (88%) with a mean age of onset of 41 years. Case reports and case series have linked a history of infection (gastroenteritis or flu-like symptoms) with idiopathic gastroparesis, and this particular subcategory is referred to as a post-transfusion general practitioner. infected. It has been previously reported that post-infectious gastroparesis accounts for about 21% of all cases of idiopathic gastroparesis. However, this number will be higher with new data. In addition, patients with post-infectious gastroparesis appear to have a higher rate of spontaneous recovery.
2. What do the studies say?
Much of the data to understand idiopathic gastroparesis comes from the NIDDK Gastroparesis Clinical Research Consortium (GpCRC), a collaborative effort from experts at several specialized academic advocacy centers in the United States. Ky. Symptoms of nausea, vomiting, and abdominal pain were associated with poor quality of life in all patients with gastroparesis. Data from the NIDDK Gastroparesis Registry showed that among 159 patients with gastroparesis (107 idiopathic gastroparesis, 52 diabetic gastropathy), nausea was the main symptom in both groups. , vomiting was more common in diabetic gastroparesis (81% vs 57% p=0.004) and abdominal pain was more common in idiopathic gastroparesis.
In addition, psychological profiles identified depression along with physical and sexual abuse present in 62% of female patients with idiopathic gastroparesis. These factors contribute to visceral hypersensitivity and may help explain the higher incidence of abdominal pain in idiopathic gastroparesis. The limited understanding of the pathogenesis of idiopathic gastroparesis has led to an inappropriate approach in the management of symptoms.
In addition, many entities (eg, scleroderma), which can cause delayed gastric emptying, may be inappropriately named idiopathic gastroparesis. Knowledge of this growing field will lead to a more focused treatment approach.
3. Pathophysiology of idiopathic gastroparesis
Although the pathophysiology of idiopathic gastric dystrophy remains unclear, several mechanisms and explanations are evolving. However, nerve function and regulation have been shown to be impaired in patients with diabetic gastroparesis, but to a lesser extent in idiopathic gastroparesis.
In addition, a role of the vagus nerve in ghrelin secretion has been suggested. Ghrelin factor is released primarily by neuroendocrine cells in the lumen of the stomach and duodenum and has been suggested to function as an appetite-stimulating hormone that acts centrally through the afferent pathway. dethrone. Ghrelin has also been shown to stimulate gastric contraction and improve meal-related symptoms and gastric emptying (gastric emptying) in patients with idiopathic gastroparesis.
Biopsy of the entire stomach in patients with gastroparesis (compared with controls) showed that nNOS expression in idiopathic gastroparesis was more frequently reduced than in patients with diabetic gastroparesis (40% vs. %). However, increased connective tissue tissue is visualized in both idiopathic gastroparesis and diabetic gastropathy by electron microscopy. Cajal's interstitial cell loss (ICC) is a predominant finding in patients with both diabetic gastropathy and idiopathic gastroparesis. Present in up to 50% of cases and associated with delayed gastric emptying in diabetic gastropathy. The interstitial cells of the cajal are considered to be the source of electrical activity in the stomach, and loss of ICC attenuates and disorganizes electrical signaling leading to decreased intestinal motility.

4. Studies on differences in gastric electromyography patterns
Patients with idiopathic gastroparesis have a more irregular pattern of EGG, with reduced EGG activity by 3 cycles/min (cpm), whereas patients with mechanical pyloric outlet obstruction have a marginal 3 cpm EGG pattern steady, high. In patients with idiopathic gastroparesis, clinical severity and nausea are related to immune-mediated infiltration of the myocardium. Evidence of lymphadenitis in a full gastric biopsy allows the diagnosis of idiopathic gastroparesis.
There is also an evolving role of pyloric pathophysiology in the development of gastroparesis. Loss of pyloric ICC is twice as common in the pylorus and fibrosis in the pyloric smooth muscle as three times more common in biopsies of patients undergoing gastric electrostimulation with pyloric dilation. Therefore, a unified concept is that gastroparesis has similarities with “colic pain”. In achalasia, there is both a stiffening of the esophageal muscle that causes a loss of motility, in addition to a non-dilated lower esophageal sphincter (LES) leading to an esophageal obstruction. In the general practitioner, there is depletion of enteric neurons, loss of ICCs in the smooth muscle of the sternocleidomastoid muscle, and impaired relaxation/compliance of the pyloric sphincter leading to fasting. Either of these “dual mechanisms” may be more predominant in an individual gastroparesis patient, but both need to be considered and addressed when planning treatment.
A variety of contributing factors and underappreciated entities can lead to the label “idiopathic gastric disorder”. Idiopathic gastroparesis is also a term that may be overused as an etiology of unexplained upper gastrointestinal symptoms. The diagnosis of idiopathic gastroparesis must be made rigorously, with particular attention to the interpretation of scintigraphic gastric emptying studies, where abnormality must be > 15% maintained at 4 h, not present. > 10%. Medications, especially opioids, are key factors to consider when interpreting a gastric emptying study.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Danny j. avalos, et al. Understanding the etiology and spectrum of idiopathic gastroparesis. Gastrointestinal motility and functional bowel disorders, series
22. april 2017 • volume xli, issue 4