This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International HospitalEosinophilic esophagitis (abbreviated as EoE) is an emerging chronic esophageal disease, first described in 1993, with increasing incidence and prevalence in Western countries. Accordingly, esophageal eosinophilia when exposed to high concentrations of esophageal acid when monitoring esophageal pH or in response to proton pump inhibitor therapy (PPI) is reflux esophagitis (GERD). ), while pH monitoring is normal or unresponsive to PPIs is eosinophilic esophagitis (EoE).
Abbreviated terms
EoE: Eosinophilic esophagitis: esinophilic esophagitis
GERD: Gastroesophageal reflux disease: Reflux esophagitis
IL: Interleukin: Interleukin factor
PPI: Proton pump inhibitor: Proton pump inhibitor Proton
PPI-REE: Proton pump inhibitor-responsive esophagal: Proton pump inhibitor-responsive esophagitis
Eosinophilia: eosinophils
VTQBCAT: eosinophilic esophagitis
1. Overview
Eosinophilic esophagitis (abbreviated as EoE) is an emerging chronic esophageal disease, first described in 1993, with increasing incidence and prevalence in Western countries. During the 80s and early 90s, esophageal dense eosinophilia was mainly associated with gastroesophageal reflux disease (GERD). Over the next 15 years, EoE and GERD were treated as separate entities: Esophageal eosinophilia on exposure to high esophageal acidity when monitoring esophageal pH or in response to inhibitory therapy proton pump (PPI) is GERD, while normal or unresponsive pH monitoring to PPIs is EoE.Guidelines updated in 2011 described a new pathological phenotype, proton pump inhibitor-responsive esophageal eosinophilia (PPI-REE), referring to patients who appeared to have EoE clinically, but achieved complete remission after PPI treatment. Currently, PPI-REE must be formally excluded before EoE is diagnosed, as 30-40% of patients with suspected EoE are eventually diagnosed with PPI-REE.
2. Advances in the pathogenesis of PPI-PREE . pathology
The prevailing hypothesis to explain PPI-REE is that coexisting GERD can be a priming event, allowing potential entry of food-derived allergenic molecules through damage to the epithelial barrier. caused by acids. Thus, GERD-induced epithelial damage can expose the deeper layers of the esophageal squamous epithelium to antigens that would not normally be able to penetrate the normal mucosa. This in turn can lead to easy antigen recognition by cellular antigen presentation. However, emerging evidence demonstrates that EoE and PPI-REE groups may even be more closely related as therapeutic PPIs not only restore integrity of the esophageal epithelium, but may also reduce esophageal epithelium. inflammatory pathway by downregulating gene expression of chemokine Th2 and cytokines.
3. PPIs partially restore the epithelial barrier function of the esophageal mucosa
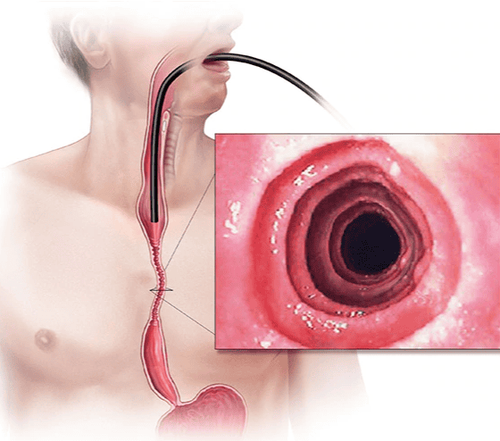
Although restoration of the esophageal epithelial barrier is the most accepted hypothesis for explaining the existence of PPI-REEs, the first study to objectively address this issue in EoE has just been published. father recently. Sixteen patients with esophageal eosinophils >15 eosinophils/field were compared with eleven controls at baseline. The integrity of the esophageal mucosa was measured in the distal esophagus, the evaluation method was using tissue impedance spectroscopy during endoscopy and histopathological examination: 2 biopsies were obtained endoscopically to Electron microscopy analysis of standard increased interstitial spacing and 4 biopsies to measure transepithelial resistance and transmucosal flux of 0.3 fluorescence labeled molecules and 40 kDa (similar to the size of a food allergen).In patients with esophageal eosinophilia, all measurements of mucosal integrity were significantly impaired when compared with controls. Patients with eosinophilic esophagitis were then given omeprazole 40 mg twice daily and reassessed 8 weeks later. Following acid suppression therapy, mucosal integrity was partially restored in PPI-REE, but not in EoE patients. The authors concluded that the deterioration of mucosal integrity in PPI-REE may be due to GERD, whereas it may be related to inflammatory cell recruitment in EoE. This study therefore suggests that exposure of the esophageal epithelium to acid reflux in PPI-REE patients, due to the barrier-depleted epithelium, may be the first 'effect' in the development of of esophageal eosinophils.
4. Could GERD be caused by cytokine-mediated damage from the Th2 immune response?
Reflux esophagitis is thought to be caused by the direct erosive effect of refluxed gastric acid on esophageal epithelial cells. In 2009, an experimental study demonstrated that GERD induces esophagitis through a cytokine-mediated mechanism rather than direct epithelial damage. In this study, the authors observed that after regurgitation surgery, the first histologically detected inflammatory response was a lymphocytic infiltration of the submucosa that progressed to the superficial mucosa. Interestingly, mucosal erosions did not appear until 4 weeks postoperatively. These findings suggest that reflux esophagitis develops primarily as a traumatic immune-related disease rather than simply a lesion. corrosive chemicals. In this regard, a recent pilot study has shown that eotaxin-3 expression in GERD and EoE cell cultures is similar when stimulated with Th2 cytokines, raising the possibility that allergic patients are at risk. In patients with EoE, reflux-induced trauma may be redirected to an alternative inflammatory pathway (Th2 immune response) than is typical of erosive esophagitis (Th1 immune response). This hypothesis would explain both the absence of features distinguishing from EoE and response to PPI therapy in PPIREE. However, more data are needed to fully appreciate this.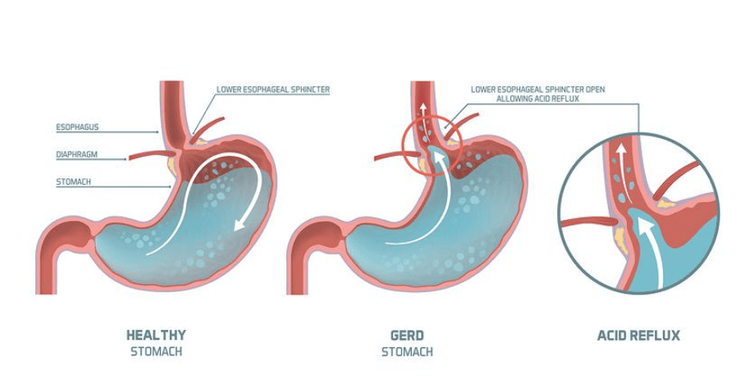
5. Effect of PPI therapy on eosinophilic esophagitis
Eotaxin-3 is a potent eosinophil chemotaxis that plays an important role in the transport of eosinophils to the esophagus in EoE. The expression of eotaxin-3 is stimulated by Th2 cytokines, such as IL-4, IL-5, and IL-13 (which are often overproduced in allergic diseases), whose effects are mediated by the transducer. signal transducers and transcriptional activators. Recent emerging translational research has demonstrated that PPIs can reduce eosinophil recruitment, independent of their acid-suppressing effects. In 2013, a pilot study demonstrated that omeprazole suppresses Th2 of cytokine-stimulated eotaxin-3 expression in esophageal squamous cell cultures from both GERD and EoE patients. The same group subsequently reported that inhibition of IL-4 and IL-13 stimulated eotaxin-3 expression in esophageal EoE cells mediated through the suppression of STAT6. When these experiments were conducted using esophageal epithelial cells cultured in vitro, PPIs observed an effect independent of their effect on gastric acid production. Overall, these later studies suggest that PPIs may have anti-inflammatory effects independent of their effect on acid secretion and cast doubt on the assumption that a positive response to PPI therapy necessarily establishes a diagnosis of GERD. . Supporting this direction of investigation, a recent study demonstrated for the first time in the laboratory that PPI therapy in PPI-REE significantly downregulates gene expression of the proximal and distal Th2 inflammatory markers. , similar to those observed in EoE patients after topical steroid administration. In addition, a recent study also showed the ability of PPI therapy for PPI-REE-associated quasi-reversible gene expression especially in relation to classical features of inflammatory allergy.Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesJavier Molina-Infante,David A. Katzka and Evan S. Dellon. Proton pump inhibitor-responsive esophageal eosinophilia: A historical perspective on a novel and evolving entity. Rev esp enfeRm dig(Madrid Vol. 107, No 1, pp. 29-36, 2015