This is an automatically translated article.
Article by Dr. Nguyen Khanh Hoa - Vinmec Stem Cell Research Institute and Gene Technology.Many gut-derived peptides have been considered as candidates for novel therapeutics for obesity and/or T2DM. However, so far, only a few have progressed to specific clinical trials.
Approaches based on other intestinal peptides
Reasons for this pretty much include concerns about efficacy, safety and/or tolerability, as well as the lack of a difference, particularly when compared to current treatments using incretin. For example, cholecystokinin (CCK), a hormone secreted by enteroendocrine cells I, received considerable attention following studies of CCK-mediated inhibition of food intake in humans. Several CCK1 receptor agonists are produced, and at least one molecule has been tested in humans in a phase 2 study. However, while inhibitory effect on gastric emptying and stimulation of contractions, Gallbladder squeeze was observed, and body weight remained unchanged even at doses that increased GI side effects, suggesting that this approach would not lead to a viable therapy for weight loss.Ghrelin is a stomach-derived hormone that has been called the “hunger hormone” because of its ability to stimulate appetite and increase food intake in preclinical and human studies. The concentration of ghrelin is highest in the fasted state and declines during nutrient consumption; Calorie restriction that occurs in the diet leads to an increase in circulating ghrelin levels and a decrease in ghrelin levels in some types of bariatric surgery. Several attempts have been made to identify the substance that affects ghrelin, its receptor and the enzyme responsible for ghrelin acylation, ghrelin-O-acyl transferase (GOAT), which has been conducted; however, molecules tested to date have failed in early-stage clinical testing due to a variety of factors, including lack of clinical weight loss significance, poor selectivity, and multiple adverse events.

Sự thềm ăn được kích thích bởi "hormon đói bụng" - Ghrelin
The potential for rapid pharmacological and physiological assessment in acute human trials by peptide infusion and the potential for additional efficacy through combination therapy make intestinal peptides suitable for evaluation as therapeutics new. The short half-life and rapid renal clearance have limited human effects, suggesting a potential role as a mediator of post-thermogenesis. Unfortunately, chronic infusion of a secretin similar to that of rats did not result in sustained loss of body weight, making it unlikely to be a therapy for weight loss (Li et al., 2018). Another interesting thing is the peptide neurotensin, an anorexia hormone whose circulating levels are corrected by bariatric surgery. Recently, long-acting neurotensin analogs have been found to inhibit food intake in rodents and, when combined with GLP-1 derivatives, reduce body weight. Neurotensin has multiple effects, including effects on the cardiovascular system, glucose metabolism, thermoregulation, and pain that may limit its usefulness; So far, no neurotensin analog has been tested in humans. Therapeutic evaluations of intestinal peptides in the past can now be remedied by peptide engineering, allowing for pharmacological evaluation in a chronic condition. These advances, coupled with increasingly sensitive methods for peptide detection and quantification, make it likely that gut-derived complementary therapy will emerge in the future.
Is the gut really the main source of intestinal peptides?
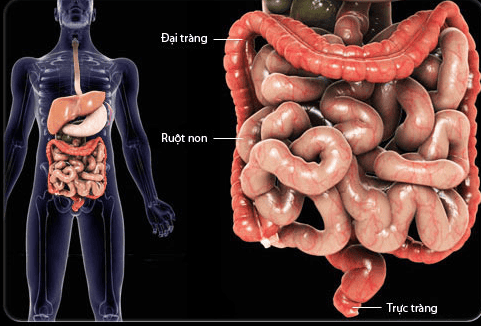
Thực tế là phần lớn GLP-1 lưu hành phần lớn bắt nguồn từ ruột
Please follow the series on “Effects of the intestine in the treatment of metabolic diseases. Drugs and Future Prospects” by Dr. Nguyen Khanh Hoa:
Part 1: Effect of gut in the treatment of metabolic diseases. Drugs and Future Prospects Part 2: Intestinal Peptide-Based Approaches Part 3: Other Enteric Peptides-Based Approaches Part 4: Is the gut really the primary source of Enteric Peptides? Part 5: Activation of Nutritional Receptors in the Intestine as a Therapeutic Strategy Part 6: Brake Inhibition: Can Somatostatin Antagonists Be Useful for the Treatment of Diabetes?