This is an automatically translated article.
The article was written by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.Autoimmune pancreatitis is an uncommon cause of chronic and recurrent pancreatitis. It occurs either as a primary autoimmune process of the pancreas or as a secondary component of a systemic autoimmune disorder.
1. Classification of autoimmune pancreatitis
There are two subtypes of autoimmune pancreatitis. Type 1 is commonly seen in elderly men and is associated with systemic disease affecting extra-pancreatic organs such as the bile ducts, kidneys, lymph nodes, and salivary glands.Autoimmune pancreatitis type II is usually seen a decade before type I. It is not sex-predominant, is not associated with other organs except inflammatory bowel disease, and is not associated with elevated IgG4 levels. . Both subtypes demonstrated lymphocytic infiltration on histological examination.
Diagnosis of autoimmune pancreatitis requires a high index of suspicion and a multimodal approach involving serologic testing, radiographic imaging, endoscopic imaging with tissue sampling, and sometimes surgical biopsy .
2. Manifestations of autoimmune pancreatitis
Autoimmune pancreatitis manifests in a variety of ways. Painless obstructive jaundice is observed in about 70% of patients. One third of patients reported loss of appetite, abdominal pain and weight loss. People with a family history of pancreatitis have an increased risk of developing the disease.3. Treatment of autoimmune pancreatitis
Autoimmune pancreatitis is treated with corticosteroids, usually starting with 40 mg/day of prednisone daily for four weeks.The patient's clinical condition was then re-evaluated and serological and radiological studies repeated. If response is appropriate, dose is tapered by 5 mg/week until completion.
Azathioprine or rituximab is used for patients with contraindications to steroids or to treat recurrent episodes.

4. The role of methods in the diagnosis of autoimmune pancreatitis
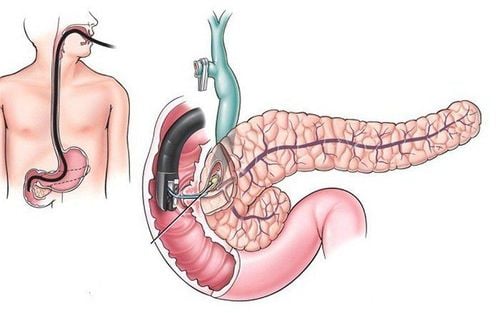
4.1 Role of blood tests and serological markers Elevated serum IgG4 is the best serological marker for autoimmune pancreatitis; however, one study reported that only 44% of patients who initially had this condition had elevated levels. Serum IgG4 may also be elevated in pancreatic cancer. The guidelines therefore confirm levels above twice the upper limit of normal as high suggestive of autoimmune pancreatitis. In addition, CA 19-9, which is normally elevated in pancreatic cancer, may also be elevated in autoimmune pancreatitis, but tends to decrease with steroid therapy. Elevated CA 19-9 suggests malignancy rather than autoimmune pancreatitis. 4.2 The role of endoscopic ultrasound biopsy Core biopsy via endoscopic ultrasound is considered the best method to obtain specimens for the evaluation of autoimmune pancreatitis.In the absence of malignant histology, biopsy specimens demonstrating lymphocytic and plasma infiltration with fibrosis support the diagnosis of autoimmune pancreatitis, particularly when plasma cells are positive for IgG4 levels. .
4.3 The Role of Other Imaging Methods Many imaging modalities have been used to assess autoimmune pancreatitis and the preferences vary by geographic region. CT, ERCP, MRCP (magnetic resonance cholangiopancreatography) and EUS endoscopic ultrasound are commonly used.
The classic findings for autoimmune pancreatitis on CT and MRCP include diffusely enlarged pancreas with a contoured cystic structure associated with diffuse hypoechoic pancreatic duct appearance.
2 - 5% of patients undergoing surgical resection for malignancy are later found to have autoimmune pancreatitis.
5. Recommendations for diagnosis and treatment of autoimmune pancreatitis
Diagnosis of autoimmune pancreatitis requires a multimodal approach Autoimmune pancreatitis should be strongly considered among the differential diagnoses in patients presenting with pancreatic adenocarcinoma Requires thorough evaluation condition to determine the most appropriate method of treatment and avoid unnecessary surgery. Autoimmune pancreatitis is a form of chronic pancreatitis. Distinguishing autoimmune pancreatitis from pancreatic carcinoma and other causes of pancreatitis remains a diagnostic challenge requiring a high index of suspicion coupled with a multimodal approach. New diagnostic criteria with increased sensitivity and specificity are needed to more clearly distinguish autoimmune pancreatitis from pancreatic carcinoma and to reduce morbidity and mortality.Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.