This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
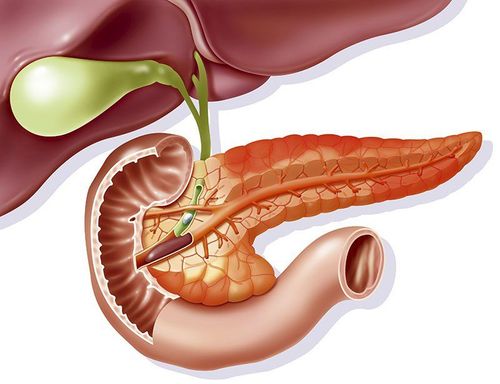
Isolated organ autoimmune disorders, formerly known as autoimmune pancreatitis (AIP), autoimmune cholangitis, and autoimmune sclerosing cholangitis, are now considered organ-specific manifestations of disease associated with systemic immunoglobulin G4 (IgG4-RD). Autoimmune pancreatitis and IgG4-RD are characterized by elevated serum IgG4 (Ab) antibody levels, accumulation of IgG4-expressing plasmacytes in affected organs, and multi-organ involvement.
It is well established that an enhanced IgG4 Ab response is a marker of autoimmune pancreatitis and that IgG4-RD for diagnosis and monitoring of disease activity. However, a significant portion of patients with autoimmune pancreatitis and IgG4-RD who develop chronic sclerosing inflammatory responses have normal serum levels of this IgG.
1. Immunoglobulins as biomarkers in autoimmune pancreatitis and IgG4-RD
Diagnosis of autoimmune pancreatitis and IgG4-RD is based on detection of elevated serum IgG4 Ab levels as well as characteristic pathological findings, including multiple infiltration of IgG4-expressing plasma cells. , storiform fibrosis, and obstructive phlebitis. Therefore, serum IgG4 Ab levels are widely used as a biomarker for the diagnosis of autoimmune pancreatitis and IgG4-RD. Furthermore, serum IgG4 levels decreased rapidly after induction of remission by prednisolone.
2. Serum IgG4 Ab levels in patients with autoimmune pancreatitis
Serum levels of IgG4 Ab in patients with autoimmune pancreatitis and IgG4-RD were much higher than in subjects with chronic alcoholic pancreatitis and in healthy controls in the authors' previous study. Therefore, it is certain that the measurement of serum IgG4 Ab levels in clinical practice is necessary not only for the diagnosis of autoimmune pancreatitis and IgG4-RD but also for the assessment of disease activity. However, Ab IgG4 levels are not always informative for the diagnosis or assessment of disease activity in these patients. Approximately 20% of patients with autoimmune pancreatitis have normal serum IgG4 Ab levels. Furthermore, a significant portion of pancreatic cancer patients also have elevated levels of IgG4 Ab. Furthermore, disease flares are sometimes seen in patients with autoimmune pancreatitis and IgG4-RD, even against the background of normalized serum IgG4 Ab levels
2.2 IgG1 Ab contributes to autoimmune pancreatitis and IgG4-RD These studies performed by Shiokawa et al strongly suggest that IgG1 Ab rather than IgG4 Ab contributes to the process. immunogenicity of autoimmune pancreatitis and IgG4-RD. Consistent with this opinion, serum levels of both IgG1 and IgG4 Abs were significantly higher in patients with autoimmune pancreatitis and IgG4-RD than in subjects with chronic alcoholic pancreatitis or in healthy controls. Strong
2.3 No significant difference in serum IgG3 Ab levels in patients with autoimmune pancreatitis For other IgG subtypes, no significant difference in serum IgG3 Ab levels in patients with autoimmune pancreatitis and IgG4-RD compared with patients with chronic alcoholic pancreatitis or in healthy controls. Serum levels of IgG2 Ab were significantly lower in patients with autoimmune pancreatitis and IgG4-RD than in patients with chronic alcoholic pancreatitis. In contrast, another report showed elevated serum IgG2 Ab levels in patients with IgG4-RD disease. This difference may be explained by the difference in the organ distribution of IgG4-RD. Serum levels of this IgG subclass are preferentially elevated in patients with orbital IgG4-RD, but not in patients with pancreatic IgG4-RD.

3. IgG levels in patients with autoimmune pancreatitis and IgG4-RD
Serum total IgG levels are also increased in patients with autoimmune pancreatitis and IgG4-RD. Therefore, elevations in serum levels of both total IgG and IgG4 are prominent features of patients with autoimmune pancreatitis and IgG4-RD. In contrast to increased levels of IgG and IgG4, serum IgM and IgA levels decreased in patients with autoimmune pancreatitis and IgG4-RD. Furthermore, the serum IgM concentration is inversely correlated with the concentration of IgG and IgG4. The diagnostic value of reducing serum IgA and IgM levels needs to be determined in future studies.
Often observed concomitant autoimmune pancreatitis/IgG4-RD and allergic disorders. In fact, serum IgE levels in patients with autoimmune pancreatitis and IgG4-RD were significantly higher than in subjects with chronic alcoholic pancreatitis and in healthy controls. This raises the possibility that serum IgE levels could be used as biomarkers for autoimmune pancreatitis and IgG4-RD. Consistent with this opinion, approximately 50% of patients with autoimmune pancreatitis and IgG4-RD exhibit increased serum IgE levels. Furthermore, changes in serum IgE levels have been associated with recurrence of these disorders. Thus, serum IgE levels can be used as a biomarker to diagnose and predict relapse in autoimmune pancreatitis, and IgG4-RD Immune autoantibodies are biomarkers in inflammation. autoimmune pancreas and IgG4-RD. Although autoimmune pancreatitis and IgG4-RD are considered to be caused by an autoimmune response, the auto Abs responsible for the development of autoimmunity have not been identified. Recently, three different types of auto Abs have been identified. These autolAbs recognize laminin 511, annexin A11 and galectin-3. Fifty-one percent of autoAb-positive autoimmune pancreatitis patients were resistant to laminin 511-E8, a truncated variant of the extracellular matrix protein laminin 511. Furthermore, serum IgG1 was purified from patients with autoimmune pancreatitis. colocalized immunity with laminin 511 in the pancreas of neonatal rats upon passivation. Huber et al. have identified annexin A11, a calcium-dependent lipid-binding protein, as a candidate autoantigen in autoimmune pancreatitis.
IgG1 auto Abs play a pathogenic role in the development of autoimmune pancreatitis and IgG4-RD. Interestingly, annexin A11 specifically IgG4 and IgG1 Abs purified from patients with shared antigenic epithelium of autoimmune pancreatitis and IgG4 auto Abs inhibits the pathogenic binding of IgG1 Ab to the divided epithelium. shall. These data suggest that IgG1 auto Abs rather than IgG4 auto Abs play a pathogenic role in the development of autoimmune pancreatitis and IgG4-RD. Confirmation of these results awaits future studies addressing the diagnostic utility of these autoAns in a large number of patients with autoimmune pancreatitis and IgG4-RD. However, the identification of autoAns involved in autoimmune pancreatitis and IgG4-RD strongly supports the idea that these disorders arise from autoimmune responses.
To have more knowledge about immunoglobulins and immune antibodies, visit vimec.com regularly and make appointments with leading doctors and experts when you need advice.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.