This is an automatically translated article.
Article by Master, Doctor Vu Duy Dung - Doctor of Neurology - Department of General Internal Medicine - Vinmec Times City International Hospital
Compressive mononeuropathy represents a common reason for a primary physical or outpatient neurologic exam. The most common of these, carpal tunnel syndrome, involves chronic compression of the median nerve. Carpal tunnel syndrome is present in up to 42% of workers in certain occupations (eg, poultry processing) and has an annual incidence of 193/100,000 in all women. Its prevalence in the US is estimated at 50/1000 people, at a cost of US$30,000 per patient. Morton's neuroma, ulnar neuropathy, paresthesia femoral pain, and radial neuropathy are the most common other peripheral mononeuropathy.
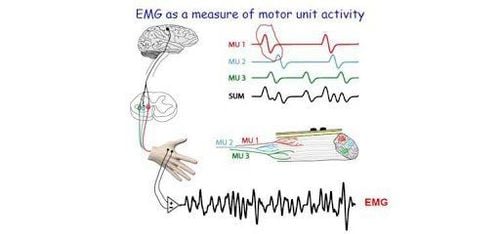
Knowledge of peripheral nerve anatomy and function allows clinical localization and subsequent further localization and confirmation by electrodiagnostic exploration and peripheral nerve imaging. In patients with mononeuropathy, etiology, severity, rate of spontaneous recovery, and patient preference are important factors in guiding treatment. Early diagnosis and effective treatment of mononeuropathy are critical to improving patients' quality of life and reducing treatment costs.
This article presents a number of nerve compression diseases of the lower extremities, with a focus on relevant anatomy, clinical symptoms, diagnostic methods, and treatment recommendations. The pathophysiological processes involved in peripheral nerve injury and compression are not covered in this paper.
Any peripheral nerve can be compressed. Some uncommon lower extremity peripheral nerve compression syndromes will be presented here.

1. Carpal tunnel syndrome
The tibial nerve originates from the sciatic nerve and receives innervation from the L4 to S1 roots. The tibial nerve separates from the sciatic nerve at the popliteal fossa and descends below the arch of the soleus. Its branches supply the plantar flexors of the ankle and to the calf nerve. At the ankle, it passes through the tarsal canal before dividing into terminal branches, the medial plantar nerve, and the lateral plantar nerve. The tarsal canal is a space between the flexor tendon and medial ankle that contains the tibial nerve, the posterior tibial artery, the posterior tibial vein, the long flexor of the big toe, the posterior tibialis, and the long flexor of the toes. The medial and lateral plantar nerves innervate skin sensation on the plantar surface of the foot, and distribute to the intrinsic muscles of the foot. The tarsal canal is a potential site for entrapment of the tibial nerve.
Carpal tunnel syndrome, also known as tarsal tibial nerve disease, is a controversial topic in neurology. In the majority of cases, the diagnosis is confirmed by clinical presentation, although diagnostic criteria are not well defined. Symptoms include numbness and painful paresthesias in the heel, inner ankle, and sole of the foot, although some definitions include ankle pain with heavy lifting. A Tinel sign may be present on the tibial nerve at the ankle. In the author's experience, idiopathic tarsal tunnel syndrome is rare. Potential causes of tibial nerve disease of the ankle include trauma, mass, accessory muscles, skeletal malformations, vascular malformations, and physician-induced causes.
Electrodiagnostic exploration may be useful to rule out other causes of carpal tunnel symptoms, but its actual effect in diagnosis is unknown. There is no single electrodiagnostic protocol, as it is often said that plantar nerve responses are often unobtainable in asymptomatic individuals, especially the elderly. A systematic review of the literature from 1965 to 2002 found only four studies that qualified for the review, and these had only group III evidence. The review concluded that nerve conduction testing could be diagnostically useful. Neuromuscular ultrasonography can help evaluate the structural causes of the symptoms of carpal tunnel syndrome, and some reports identify cross-sectional threshold values used in the diagnosis of the syndrome. spontaneous ankle.
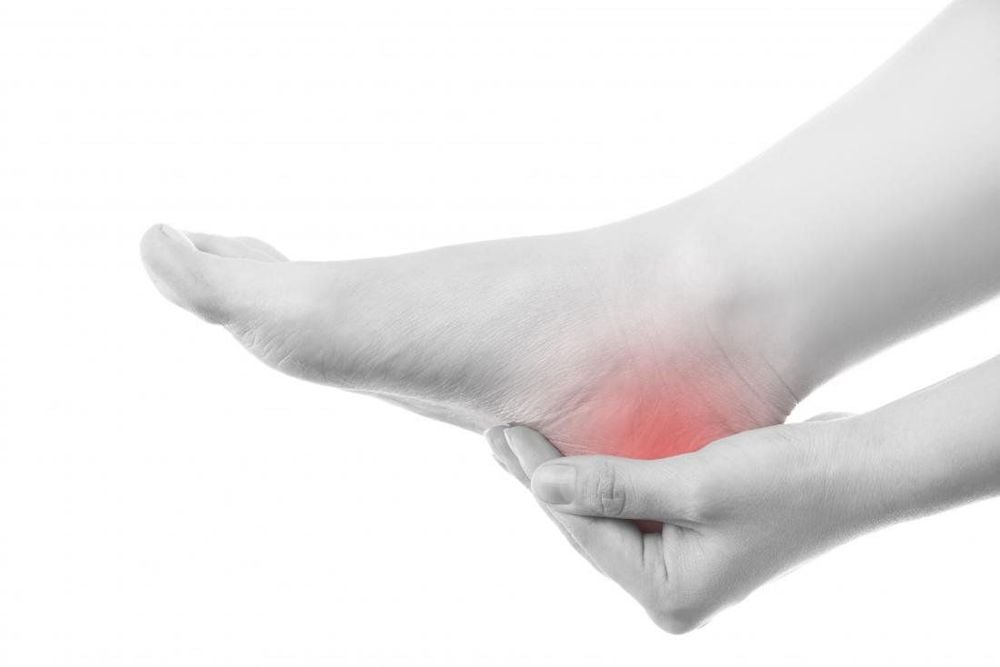
If there is no structural cause of compression, the true value of surgical decompression is unknown. A 2015 review of 31 patients surgically treated for tarsal tunnel syndrome found a good outcome in 71% but found only 6 out of 11 patients with idiopathic tarsal syndrome to improve. The best surgical outcomes are seen in patients with an identifiable cause for tarsal tunnel syndrome, including trauma and mass crowding. This should be considered when planning treatment.
2. Morton's neuroma
Although a separate entity from the tarsal tunnel syndrome, Morton's neuroma is a monotypic disease of the distal tibial nerve presenting with throbbing pain in the toes and other associated paresthesias in the anterior part of the foot. Legs appear when carrying heavy loads. It results from chronic recurrent mechanical trauma to the plantar fascia nerve and is thought to result from degenerative perinerveal fibrous hypertrophy, as opposed to true neuroma. The most common site is the third or fourth interphalangeal nerves. Diagnosis is through physical examination and, more recently, ultrasound.

3. Paresthesia thigh pain
Paresthesia femoral pain is the term commonly used to describe the pathology of the lateral femoral cutaneous nerve. The lateral femoral dermal nerve originates from the L1 to L3 roots and the lumbar plexus and is a single sensory nerve. It travels above the pelvic muscles and below the inguinal ligament, so it has a tendency to get injured and compressed. The lateral femoral cutaneous nerve can have a different pathway between individuals, with five distinct morphologies identified, making diagnostic testing and treatment challenging.
Paresthesia thigh pain is associated with obesity, diabetes, and tight clothing. Other causes include trauma and surgical damage. Typical symptoms of paresthesia thigh pain include paresthesia and loss of sensation on the lateral or anterolateral aspect of the thigh. Pain can be severe and is described as stabbing, stabbing, or burning. Physical examination will reveal sensory loss according to the distribution of the lateral femoral cutaneous nerve without accompanying findings suggestive of lumbar radiculopathy or lumbar-sacral plexus disease. Electrodiagnostic exploration is useful not only in diagnosis but also to rule out other causes. Neuromuscular ultrasonography may be useful in guiding electrode placement to examine the lateral femoral cutaneous nerve and to locate localized nerve hypertrophy.
Treatment of paresthesia thigh pain is usually conservative, including behavioral changes (eg, wearing looser clothing), symptomatic relief of paresthesias with nonsteroidal anti-inflammatory drugs, and nerve block. Investigation and surgical treatment should be considered as a last resort if there is no mass lesion.
Currently, Vinmec International General Hospital has implemented surgery for nerve compression diseases. In particular, with the pioneering of electrical diagnostic techniques. Vinmec is one of the few addresses that deploys specialized techniques, with modern equipment of NATUS (USA), the specialist doctor after performing the examination, recording and reading the results will provide a method to diagnose the disease. accurately, giving patients a chance to recover, safe treatment and no complications.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Hobson-Webb LD, Juel VC. Common Entrapment Neuropathies. Continuum (Minneap Minn) 2017;23(2, Selected Topics in Outpatient Neurology):487-511.