This is an automatically translated article.
The article was professionally consulted with Master, Doctor Nguyen Minh Son - Interventional Cardiologist - Department of Medical Examination & Internal Medicine - Vinmec Nha Trang International General Hospital.Severe heart failure is a complex clinical syndrome that results from physical damage or dysfunction of the heart leading to an inability of the ventricles to receive blood (diastolic heart failure) or eject blood. (systolic heart failure). Currently, medicine has many solutions to treat heart failure patients, including patients with severe heart failure. Digoxin drug treatment of heart failure has been interested in recent times. The following article will provide some precautions when using Digoxin to treat severe heart failure.
1. Objectives and principles in treatment regimens for severe heart failure
Chronic heart failure is a chronic disease that requires lifelong management. With treatment, however, the signs and symptoms of heart failure can improve, and sometimes the heart becomes stronger, and heart function recovers. The right treatment can help people have a better quality of life, live longer, and reduce the risk of sudden death. In most cases of heart failure, doctors will use a combination of medications or assistive devices.To treat heart failure, doctors will combine drugs depending on the symptoms, stage and cause of heart failure will have different drug regimens.
Treatment goals for severe heart failure: Immediate goal (emergency room/ICU)
Improve hemodynamics and organ perfusion. Restore blood oxygenation. Reduce symptoms. Limit damage to the heart and kidneys Prophylaxis of venous thromboembolism. Reduce recovery time. Immediate goal (in hospital)
Identify cause and comorbidities. Adjust therapy to control symptoms and congestion and optimize blood pressure. Initiate and gradually increase the optimal therapeutic dose. Consider instrumental therapy in suitable patients. Pre-discharge and long-term management:
Planning of care provided: Schedule dose adjustment and treatment monitoring. Necessity and timing of treatment with assistive devices Who will examine and monitor the patient and when. Incorporate disease management, education, and lifestyle changes. Prevention of early re-hospitalization. Improve symptoms, quality of life and survival. Cardiovascular intensive care unit admission criteria: Intubated patient/intubated patient. Signs/symptoms of hypoperfusion are present. SpO2 < 90% despite oxygenation. Using accessory respiratory muscles, respiratory rate > 25l/min. Heart rate < 40 or > 130/min, systolic blood pressure < 90 mm Hg.
Cơ chế tác dụng của thuốc Dogoxin
Some principles are applied in the treatment regimen: Increase the drug dose from the lowest to the highest dose so that the patient can tolerate Some elderly patients, chronic kidney disease ... need regular checkup. , increase dose slowly Monitor vital signs before and during dose increase (postural blood pressure, heart rate, symptoms on standing, bradycardia, low systolic blood pressure) Adjust dose of each drug class Monitor kidney function, do electrolyte tests. Patients may feel tired or weak when the dose is increased. If vital signs are good, these symptoms should resolve within a few days Do not stop treatment abruptly Diuretic and salt restriction at signs of fluid retention Beta-blockers (Bisoprolol, Carvedilol, Metoprolol succinate, Nebivolol) used in All cases except contraindications Ivabradine alone or in combination with beta-blockers when heart rate > 70 beats/min Angiotensin II receptor blockers, ACE inhibitors alone or in combination with Digoxin Avoid antiarrhythmic drugs, antiarrhythmic drugs non-steroidal inflammation or COX-2 inhibitor, calcium channel blocker Combination ACE inhibitor, Beta blocker and Hydralazine plus Nitrates Aldosterone antagonists: Spironolactone, Eplerenone
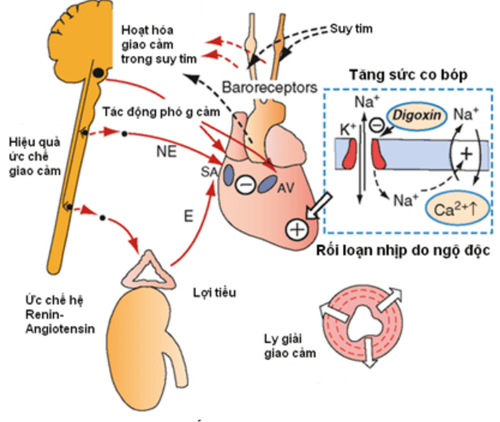
2. Digoxin in the treatment of heart failure
Digoxin is an old drug but has a rather sophisticated and quite modern pharmacological structure. It is the only oral inotropic agent. And also a diuretic.Digoxin, if it is effective, has some distinct advantages over existing heart failure medications. Provided that toxicity is avoided, digoxin has no side effects. Unlike other heart failure interventions, with the exception of cardiac resynchronization therapy, digoxin increases systolic blood pressure. Low arterial pressure is a poor prognostic sign. Because renal autoregulation in people with heart failure is faulty, a decrease in arterial pressure can impair renal function. Unlike ACE inhibitors and aldosterone antagonists, digoxin does not worsen renal function. Unlike β-blockers, it does not cause fatigue, and although the evidence that digoxin improves quality of life is not strong, the evidence for β-blockers is also not strong.
Trials have shown that digoxin reduces heart rate, increases systolic blood pressure and ejection fraction, and improves symptoms, all of which help predict a better prognosis. It also improves quality of life, at least in the short term. In fact, digoxin improves prognostic predictors but has not been shown to improve prognosis. In addition, it has been shown that there may be antagonistic adverse effects, such as hypokalemia, arrhythmia, death, etc., when used in high doses.

Thuốc digoxin được sử dụng trong điều trị bệnh lý tim mạch
Optimal Digoxin Dosing The mean maintenance dose of digoxin in the DIG Study was 0.25 mg daily - 70% of patients were maintained Steady-state serum digoxin levels in patients receiving this dose (available in a small number of patients) averaged from 0.8 ng/mL to 0.9 ng/mL. treatment range 0.5–2.0 ng/mL. Higher maintenance doses of digoxin (0.375 mg daily) were used in the PROVED and RADIANCE trials, but there was no evidence for an increase in the dose. in the range of 0.2–0.39 mg daily leading to symptom improvement There is some evidence that the risk of digoxin toxicity (including death) increases rapidly when the mean daily digoxin dose exceeds 0, 25 mg per day or c when the serum digoxin concentration is above 1.0 ng/mL.
It is especially important to use lower maintenance doses of digoxin (0.125–0.25 mg/day) in the elderly because of age-related decline in renal function. This problem is likely to arise frequently in clinical practice, as the elderly make up the majority of the heart failure population. Furthermore, digoxin toxicity can be difficult to discern in the elderly. Concomitant administration of drugs that increase serum digoxin concentrations (eg, amiodarone, quinidine, verapamil) may also require a reduction in the maintenance dose. Caution also applies to the use of certain herbal preparations and so-called supplements in patients taking digoxin. For example, squill, strophanthus and oleander contain cardiac glycosides and can trigger toxicity, while senna and cascara can increase potassium loss, leading to toxicity, and St John's wort reduces serum digoxin levels by about 25%.
3. Application of Digoxin in clinical treatment of severe heart failure
Heart failure with atrial fibrillation: digoxin is indicated. Sinus arrhythmia: Since digoxin was long suspected to be ineffective and limited its use, the value of digoxin in the treatment of heart failure with sinus rhythm was re-established based on evaluations of multiple studies. blind and discontinuation studies. Whether to use digoxin or not also depends on each case such as: + Mitral stenosis with sinus rhythm does not require digoxin unless there is already right heart failure.+ Digoxin is not beneficial for patients with left ventricular hypertrophy, the ejection fraction is still good, even harmful if the left ventricle is very thick because when the heart muscle contracts, it will increase the obstruction on the ejection path to the left ventricle. .
+ Congestive heart failure due to factors such as anemia, hyperthyroidism, infection only need to give digoxin temporarily initially, not long-term maintenance.
Heart failure due to ischemic heart disease: when using digoxin, myocardial oxygen demand will increase or decrease depending on two opposing factors: decreased wall tension and increased myocardial contractility. Digoxin can also relieve symptoms of angina if the heart is enlarged and congested. However, if the heart is already very dilated, the response to digoxin may change. Digoxin also has the potential to aggravate myocardial ischemia by increasing oxygen demand unless this adverse effect is masked by a decrease in ventricular size and a decrease in cardiac wall tension. A combination of digoxin and a beta-blocker has also been found to be beneficial in patients with angina, cardiomegaly, and impaired systolic function.
Acute myocardial infarction: digoxin can constrict coronary arteries and increase the size of the infarct area. If there is atrial fibrillation with rapid ventricular response, esmolol or verapamil, diltiazem should be used.

Người bệnh cần được điều trị suy tim theo phác đồ của bác sĩ chuyên khoa
Corrupted mind: digoxin not only offers many benefits, but can sometimes have the opposite effect. Although digoxin can increase cardiac output, it can increase pulmonary artery pressure, not to mention the risk of digoxin toxicity due to O2 deficiency and electrolyte disturbances. In contrast, if right heart failure is a consequence of left heart failure, digoxin is indicated.
4. Notes when using Digoxin in clinical treatment of severe heart failure
The daily dose of digoxin depends on renal function as assessed by BUN or serum creatinine. However, in the elderly, creatinine can be normal even though the glomerular filtration rate is reduced to 50% if the patient is exhausted, the muscle mass is low, so the creatinine release is also low. In addition, low weight makes digoxin less attached to muscle fibers, so the concentration of digoxin in the blood increases, easily causing poisoning. The dose of digoxin in the elderly is 0.125 mg/day, although 0.25 mg/day can be used if creatinine is - 1.5 mg%.The problem with digoxin is that the therapeutic dose and the toxic dose are very close to each other. May be partially based on digoxin/blood concentrations provided blood is not drawn too early <6–8 h after oral dose and <4 h after parenteral dose. Therapeutic concentration is 1-2ng/ml. However, digoxin toxicity can still occur with digoxin/blood concentrations within therapeutic limits if the patient's serum potassium is low. If the patient is taking quinidine, amiodarone, digoxin concentrations are often doubled while other antiarrhythmic drugs such as procainamide, disopyramide, lidocaine, sotalol, beta-blockers do not affect the pharmacokinetics of digoxin. Verapamil increases digoxin levels while diltiazem has little effect.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.













