This is an automatically translated article.
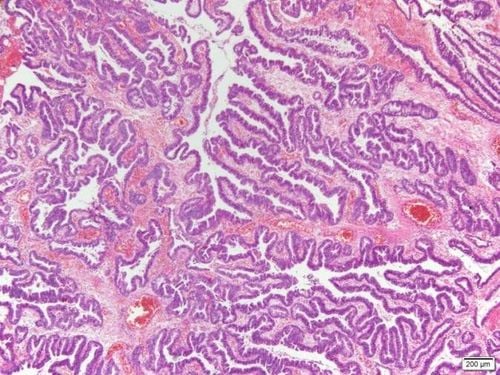
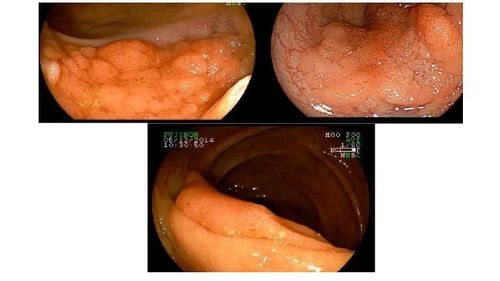
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.In recent years, nonpolyposis colorectal tumors (sessile polyps) and especially lateral spread tumors (LSTs) are becoming a huge concern. These lesions have a higher frequency of high-grade dysplasia (HGD) and are more locally invasive than nodules of the same size.
1. Classification of non-polyposis colorectal tumors
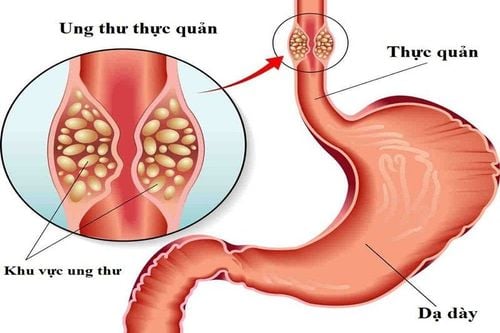
Colorectal cancer is a major health problem, it is the second most commonly diagnosed disease in women and the third in men.
In recent years, pedunculated colorectal tumors and especially lateral spread tumors (LSTs) are becoming a huge concern. LST is a large flat neoplasm that tends to grow longitudinally on the surface of the intestine.
By definition, LST indicates a diameter exceeding 10 mm. LSTs and large sessile polyps have a higher incidence of high-grade dysplasia (HGD) and are more locally invasive than nodules of the same size. This is often a technical challenge for the endoscopist both in terms of diagnosis and resection. That is why the term “advanced mucosal neoplasm” (sessile neoplasm) has been proposed recently for these two types of lesions.
2. Treatment of non-polyposis rectal tumors 2.1. Endoscopic treatment Given the above characteristics (appearance, pith and vascular shape) as well as the anticipated risk of submucosal invasion, the indication for appropriate therapy should be carefully considered.
Lesions suitable for endoscopic resection are those that are confined to the mucosa (or the superficial layer of the submucosa in select cases), whereas deeper invasion makes endoscopic therapy scan is not feasible.
Over the years, several excision techniques for the treatment of polyps have been described, among which endoscopic mucosal resection and resection (EMR) is the most common. More recently, endoscopic submucosal dissection (ESD) has been developed to improve the "micromass" resection rate of polyps.
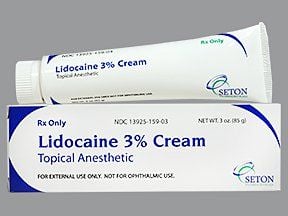
2.2. Solutions used for submucosal injection Saline is the most commonly used injectable solution worldwide. Submucosal epinephrine saline injection has been shown to be an effective method for complete endoscopic polypectomy, particularly in flat or pedunctal lesions, and is widely used because of its simplicity and cost. low and widely available. On the other hand, some studies have raised concerns about its effectiveness in preventing postoperative bleeding, which is caused by the short period of mucosal elevation following epinephrine injection.
Therefore, other agents (such as sodium hyaluronate, hydroxypropyl methylcellulose and glycerol) were tested for their ability to form a longer-lasting submucosa due to their viscous properties. In doing so, these agents allow for longer procedures and increase tumor resection rates, even for large lesions. However, despite the promising results of the aforementioned reports, their effectiveness in preventing bleeding after gastrointestinal polypectomy (PPB) remains controversial.
The ideal solution for submucosal injection should be inexpensive, readily available, non-toxic, easy to prepare and inject, and must provide a long-lasting submucosal buffer.
Succinylation of gelatin appeared to meet these criteria in a recent randomized controlled trial that, while showing a significant improvement in efficacy, found no reduction in PPB and perforation rate after gelatin injection. submucosal compared with saline.
2.3. The injection and cutting EMR technique consists of simple predefined steps. Initially, the solution was injected into the submucosa at one edge of the lesion with a disposable needle to provide a safe submucosa buffer and better resection. While the assistant nurse injects the solution, the endoscopist will insert the needle straight into the wall of the colon. After submucosal injection, a disposable electrocautery noose is placed over the elevated tissue and gently pressed against the mucosa, while closing until resistance is felt. The lesion was then excised using a mixed current supply electrocautery unit.
Lesions larger than 20mm usually cannot be resected as a whole, therefore partial resection is required. In cases where residual tissue is suspected after resection, application of argon plasma coagulation (APC) can ablate residual areas, thereby reducing the risk of colorectal tumor recurrence.
There is no clear consensus on the prophylactic use of clips after excision of pedunculated neoplasms.
2.4. ESD technique – submucosal dissection Recent improvement of ESD tools and skills in the treatment of colorectal tumors as an alternative to EMR. While in other areas of gastrointestinal endoscopy, ESD has been shown to be superior to EMR, however, indications for colorectal ESD are relatively few, even in experienced centers because most Most colorectal tumors are benign and can be resuscitated by partial EMR with minimal risk of recurrence.
In ESD, after submucosal injection, a specialized electrocautery cut around the lesion margin is performed to isolate the surrounding 3 or 4 mm normal mucosa. The submucosa submucosa was further injected and then dissected by the ESD knife through the submucosa to excise the en mass lesion.
In summary, EMR (partial for LST > 20 mm, mass for smaller tumours) remains first-line therapy for sessile colorectal tumors. ESD in high-volume centers or surgery should be considered for large LSTs where total mass resection is required and cannot be achieved by EMR.
2.5. Follow-up management after pathology of polyps If the pathological analysis of the specimen reveals the presence of adenocarcinoma and the lesion is limited to the mucosa (referred to as “carcinoma”) tissue in situ"), there is no indication for surgery provided that laparoscopic resection is radical. In contrast, adenocarcinomas that invade the submucosa have a risk of lymph node metastasis of 6-12%, so in Western countries they are often indicated for colectomy.
As further studies have shown, well-differentiated adenocarcinoma with submucosal invasion within 10mm without lymphatic or vascular involvement carries a small risk of lymph node metastasis, otherwise want to say no. In Japan, sessile polyps with these features are treated by endoscopic resection.
Bleeding, abdominal pain, and perforation are the most common and serious complications, especially after laparoscopic sessile resection. All of these adverse events are reported more frequently after ESD, therefore this technique should only be considered in highly experienced centres.
3. Follow-up after treatment for pedunculated colorectal tumors The follow-up recommendations for pedunculated colorectal tumors are exactly the same as those with regard to pedunculated polyp lesions.
After partial EMR, a follow-up colonoscopy should be performed at 3 months to assess the completeness of resection and to remove any residual or recurrent lesions. If a residual or recurrent lesion is recognised, it should be treated accordingly. Once complete resection has been established, subsequent monitoring should be individualized based on the endoscopist's assessment.
In the case of tumor resection, surveillance colonoscopy should be scheduled after 3 years for adenomas ≥ 1cm or with villus features, high grade dysplasia (regardless of size).
Usually, less intensive follow-up (colonoscopy at age 5-10) is needed in cases of single pedunculated polyp <1 cm presenting with tubular features or low-grade tissue dysplasia learn.
However, in real life, in certain cases (such as unclear radiculopathy, need for argon treatment after resection, the resected margin is determined by the pathologist as cannot be assessed), monitoring can be even more stringent.
4. Conclusion Stemless polyps are commonly found during screening colonoscopy and present a diagnostic and therapeutic challenge for the colonoscope, which will provide the characterization and classification of the colonoscopy. All sessile polyps were diagnosed. Staining endoscopy and NBI are useful tools for the detection of pedunculated non-polyposis lesions and should therefore be routinely used in clinical practice. The pituitary and vascular pattern features can accurately predict and assess the risk of invasive submucosal disease. EMR represents first-line therapy in cases where lesions are limited to the mucosa, while patients with superficial submucosal invasion should be offered ESD (at highly experienced Centers) or surgery. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Antonio Facciorusso et al. Non-polypoid colorectal neoplasms: Classification, therapy and follow-up. World J Gastroenterol. 2015 May 7; 21(17): 5149–5157.