This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Surveying the gut microbiome has gradually changed the understanding of esophageal disease. Analysis of intestinal microbiota imbalance will provide more detailed information on the pathogenesis of reflux esophagitis, sequelae and other related diseases.
1. Imbalance of intestinal microflora in upper gastrointestinal malignancies
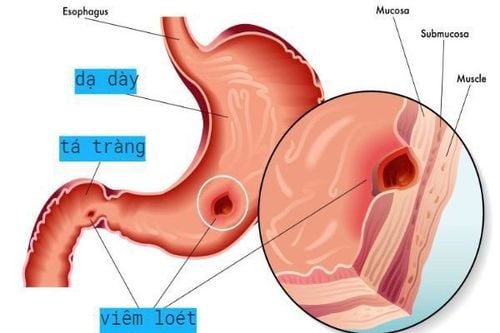
Dysbiosis - intestinal microbiota imbalance is a term that includes a change in the composition of the microbiome associated with that found in healthy individuals. When differentiating the biome of a normal healthy esophagus from dysbiotic disease states, such as reflux esophagitis, eosinophilic esophagitis, Barrett's esophagus, or adenocarcinoma of the esophagus, It is clear that biological dysregulation may precede inflammation. Therefore, the composition of the microbiome may play a large role.
2. Esophageal adenocarcinoma Inflammatory pathogenesis The pathogenesis of esophageal adenocarcinoma is thought to be due to a combination of genetic predisposition as well as environmental factors. The majority of cases are associated with environmental triggers such as smoking, obesity, and Barrett's esophagitis/reflux esophagitis. The incidence of esophageal adenocarcinoma in Barrett's esophagus is well established, although recent data suggest a lower incidence in the 0.1-0.2% range.
Role of the microbiome in adenocarcinoma of the esophagus All stages in the reflux esophagitis pathway (Barrett's esophagus, adenocarcinoma of the esophagus) have common features of part of the local flora. The change from type I to type II esophageal microflora is often associated with the initiation of inflammatory processes due to reflux. Subsequent activation of the lipopolysaccharide cascade - Toll-like-receptor 4 leads to activation of NF-kB, which further increases COX-2 production. Elevated COX-2 is associated with progression of Barrett's esophagus with high-grade dysplasia.
However, more recent data have identified relatively specific changes that are associated with progression from high-grade dysplasia of Barrett's esophagus and adenocarcinoma of the esophagus. Patients with dysplasia have an increased amount of Proteobacteria and a decreased amount of Firmicute. Notably, Streptococcus spp. was reported to be unchanged between non-dysplastic Barrett's esophagus and high-grade dysplasia/oesophageal adenocarcinoma, suggesting that the variation in Streptococcus spp. may not play a role in carcinogenesis.
The composition of the esophageal microbiota in esophageal adenocarcinoma is strongly linked to the oral cavity composition, Specifically, the oral flora such as Treponema denticola, Streptococcus mitis and Streptococcus anginosus are associated with cancer. esophageal letter. Although the overall abundance of Streptococci appears to be unchanged between Barrett's esophagus and non-malplastic esophageal adenocarcinoma, individual species may have different abundances. In addition to the pathogenic link between the oral flora and the esophagus, changes in composition that are associated with a reduced risk of adenocarcinoma are also shared. Notable was the abundance of Bifidobacteria spp., Bacteroides spp., Fusobacteria spp., Veillonella spp., Lactobacillus spp. and Staphylococcus spp. associated with the risk of adenocarcinoma. Leptotrichia spp. has been shown to be a specific genus associated with esophageal adenocarcinoma. In addition, reduction of several species, including Neisseria and Streptococcus pneumoniae, also reduces the risk of progression to cancer in the upper gastrointestinal tract.

Role of the gut microbiota in squamous cell esophageal cancer Microbiological assessment of patients with squamous cell esophageal cancer revealed specific changes when compared with healthy controls, Notably, the percentage of Actinomyces spp increased, Atopobium spp. and Fusobacterium spp. reduction. In general, there was also a decrease in bacterial diversity and an increase in inter-individual composition variability, which suggests that the dysbiotic state is not stable. For example, adenocarcinoma of the esophagus is strongly associated with oral disease/dysbiosis and squamous cell esophageal cancer. A decrease in the diversity of the oral microbiota is associated with squamous cell esophageal cancer, because the movement of bacteria throughout the body can disrupt the normal bacterial composition of the esophagus, contributing to the development of esophageal cancer. intestinal microbiota imbalance.
4. Environmental factors that contribute to dysbacteriosis Smoking is associated with many changes in the oral microbiota, some of which overlap with dysbacteriosis in squamous cell esophageal cancer. In particular, the increase in flora in the phylum Actinobacteria, genera Atopobium, Prevotella, decreased in Fusobacteria spp. reported.
Alcohol consumption can negatively affect epithelial barrier function. In addition, it may contribute to local dysbiosis through the metabolism of local flora to toxic metabolites, such as acetaldehyde. Alcohol intake was associated with reversible colonic microbiota changes with probiotics, suggesting microbiome plasticity. The combination of biogenesis and epithelial dysfunction may contribute to endotoxins and systemic inflammatory responses, which play a role in carcinogenesis. In conclusion, microbiome alterations may also play a prognostic role in squamous cell esophageal cancer. An increase in phyla Firmicutes, Bacteroidetes and Spirochaetes, and a decrease in Proteobacteria were associated with lymph node spread with Streptococcus spp. and Prevotella spp. specifically specified.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: D'Souza SM, Houston K, Keenan L, Yoo BS, Parekh PJ, Johnson DA. Role of microbial dysbiosis in the pathogenesis of esophageal mucosal disease: A paradigm shift from acid to bacteria? World J Gastroenterol 2021; 27(18): 2054-2072 [DOI: 10.3748/wjg.v27.i18.2054]