This is an automatically translated article.
The article is professionally consulted by Doctor Nguyen Van Duong - Cardiovascular Center - Vinmec Central Park International General Hospital.
Chest pain is a common symptom that makes patients feel anxious and compulsive to seek medical attention. Diagnosing and treating the cause of acute chest pain is potentially dangerous and can even lead to death if not detected and treated promptly.
1. Recognizing acute angina
Acute angina pectoris caused by coronary artery disease often has a feeling of squeezing and pressure on the chest, although the pain may not be as typical as just discomfort in the left chest (common in adults). elderly or female). Chest pain that feels like a tear in the chest, spreads from the front of the chest to the back or from the back to the front, suggesting aortic dissection. Sharp stabbing chest pain is usually due to pulmonary or pleural or musculoskeletal causes. Burning pain, dyspepsia thought of gastrointestinal causes.Pain associated with physical activity suggests myocardial ischemia, pain that increases at rest suggests acute myocardial infarction (MI). Sudden onset of pain may suggest aortic dissection, pulmonary infarction, or pneumothorax. Burning pain that appears after eating suggests digestive diseases.
Time of onset of pain: pain is quick for a few seconds and then goes away on its own or mild pain lasts for many days rarely due to dangerous causes. Pain that comes on suddenly or appears on exertion and lasts more than 15 minutes suggests dangerous causes such as myocardial infarction, aortic dissection.
Pulmonary symptoms: chest pain accompanied by vomiting, nausea, sweating, syncope and shortness of breath is often a dangerous cardiovascular disease. Severe pain with hemoptysis may indicate pulmonary infarction , lobar pneumonia , lung abscess or tuberculosis .
Đau cấp ngực có thể báo hiệu của bệnh nhồi máu cơ tim
2. Causes of dangerous chest pain you need to pay attention to
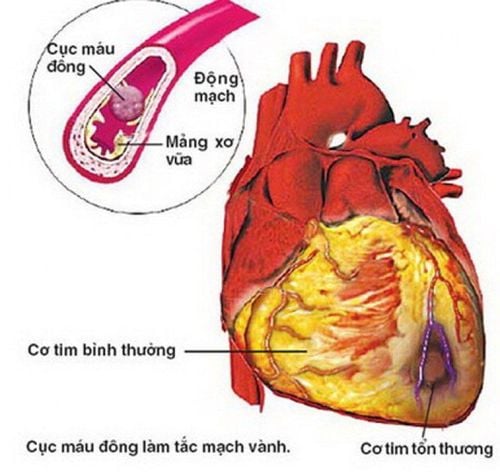
Heart attack and unstable angina A heart attack occurs when an artery that supplies blood to the heart (coronary artery) is blocked. The patient may have a previous history of chest pain or a previous diagnosis of angina.Characteristic chest pain usually pain in the left anterior region of the heart, a feeling of heaviness or tightness in the chest, typical pain may radiate to the neck, shoulder or inner arm. The pain usually lasts more than 20 minutes. Pain can occur spontaneously or after exertion such as walking, climbing stairs, strong emotions... if the patient has a pre-diagnosed patient, the pain can be relieved after taking a nitroglycerin tablet, if sucking nitroglycerin does not help the patient may have had a real heart attack. Patients with suspected acute myocardial infarction should be hospitalized to confirm the diagnosis and treat as soon as possible.
Aortic dissection The aorta is the main artery originating from the heart that carries blood throughout the body, aortic dissection is when the lining of the aorta is torn and dissected along the arteries leading to ischemia organs or rupture of the aortic aneurysm causing hemorrhagic shock.
Characteristics of aortic dissection patients often have very severe chest pain, pain radiating to the back, may show signs of anemia, and if blood pressure is measured, blood pressure readings may be different in both arms.
Dissection of the ascending aorta is a cardiovascular emergency that requires immediate diagnosis and management because it is life-threatening.
Pulmonary embolism is a blockage of one of the main blood vessels that supply blood to the lungs. This is the cause of chest pain that can be life-threatening.
Symptoms are often varied, can include chest pain, shortness of breath, low blood pressure, coughing up blood. Pulmonary embolism should be considered when these symptoms can occur suddenly, especially in patients with prolonged bed rest, in patients with cancer, or in patients with associated painful swelling of one leg.
Acute cardiac tamponade This is a condition in which pericardial fluid (the pericardium is a sac formed around the heart) presses on the heart, preventing the heart from contracting. Patients often feel constant pain, feeling like suffocating chest, may have pulse collapse, cyanosis...
3. Subclinical diagnosis of acute chest pain
The most important tests: electrocardiogram, cardiac enzymes, echocardiography and straight chest X-ray.Electrocardiogram: + The ECG should be recorded for all patients with chest pain.
+ Diagnose immediately if there are electrocardiographic manifestations of acute coronary syndrome (unstable chest pain and myocardial infarction), arrhythmic manifestations or not.
+ Pericardial effusion usually presents with low voltage or respiratory voltage variation (QRS alternance).
+ Large pulmonary infarction often presents with acute cor pulmonale (S1Q3T3: S deep DI, deep Q Dll, deep T Dllll).
Cardiac enzymes: + Increase CK index, CK MB, CKMB/CK ratio > 10%.
+ Troponin plays an extremely important role in excluding acute coronary syndrome, specific for myocardial damage. Note that troponin must be more than 4 hours after the onset of pain to increase.
+ In addition, there is also myoglobin, LDH or GOT/GPT, but the value and specificity are not high in MI.
Other tests:
– Straight chest X-ray: effective in excluding pneumothorax or suspected aortic dissection (widening mediastinum), heart failure, pulmonary edema, bone lesions. Or sometimes diaphragmatic hernia. Mediastinal pneumothorax.
– Chest CT scan when aortic dissection or intrathoracic lesion is suspected or multi-sequence CT coronary evaluation.
– Echocardiography: Assess cardiac function, mechanical complications of myocardial infarction as well as determine whether cardiac tamponade is present. In some cases, echocardiography can show a thrombus in the pulmonary artery.

Chụp CT giúp chẩn đoán đau cấp ngực
4. Management of acute chest pain
All patients with chest pain should be prioritized for immediate triage, and should be seen within < 5 minutes of patient arrival.Pain with any of the following features should be given priority:
+ There is cardiovascular disease or obvious cardiovascular risk.
+ The pain is visceral in nature.
+ There are vegetative signs (sweating, vomiting, nausea).
+ Difficulty breathing.
+ Abnormalities in pulse and blood pressure.
Rapid assessment and stabilization of vital functions. Detailed examination (history, history, detailed examination) is performed after or concurrently with the stabilization of vital functions.
+ Have an electrocardiogram monitor.
+ Record 12-lead electrocardiogram, must be viewed within 10 minutes.
+ Breathing oxygen.
+ Pain relief.
+ Place an intravenous line.
+ Take blood to test for troponin, CKMB, blood sugar, electrolytes, kidney function.
+ Considerations for:
Aspirin. Nitroglycerin. Analgesic: morphine. + Note:
If there is a right ventricular myocardial infarction should not use morphine or vasodilator drugs such as nitroglycerin. For early analgesia, use a pain scale of 0-10 points. Ask the patient to rate their own pain from 0 (no pain) to 10 (most severe pain). Monitor Sp02, electrocardiogram, measure blood pressure several times. Besides, depending on the cause, after having the subclinical results to treat in some directions:
+ With acute coronary syndrome:
Oxygen ventilation. For pain relief: morphine should be used if there are no contraindications. Place an intravenous line: draw blood for tests. Have an electrocardiogram monitor to prevent arrhythmias. Conduct MONAC regimen including morphine, oxygen, nitroglycerin, aspirin, clopidogrel. Cardiology consultation for emergency intervention. + Aortic dissection:
Pain relief. Control blood pressure and heart rate. Emergency surgery if aneurysms dissect the ascending thoracic aorta. + Pulmonary artery occlusion:
Oxygen breathing. Give early anticoagulation: heparin followed by vitamin K antagonist. Consider indications for fibrinolysis. Surgery if hemodynamic disturbances are present. + Pressure pneumothorax: emergency pleural puncture and opacification.
+ Pain in the stomach - esophagus: give antacids and coat the stomach lining.
+ Pancreatitis: gastric tube insertion, fasting, pain relief.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical professionals, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Dr. Nguyen Van Duong has many years of experience in the diagnosis and treatment of internal cardiovascular diseases and cardiovascular interventions; Perform other noninvasive functional investigations in the diagnosis and treatment of cardiovascular diseases. Currently working as a treating doctor at Cardiovascular Center, Vinmec Central Park Hospital from August 2017 aid.