This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
1. Liver damage caused by Covid-19 in special populations
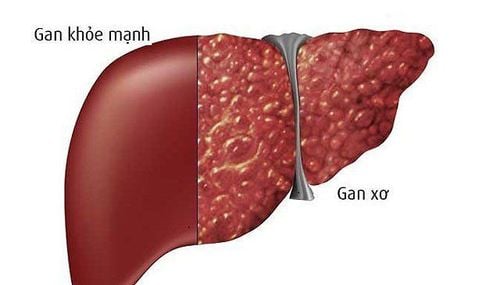
As of now, there are about 400 million CLD patients in China, including those with chronic viral hepatitis, fatty liver, alcoholic liver disease, cirrhosis or other liver diseases. Therefore, in patients with SARS-CoV-2 infection, the influence of pre-existing liver disease on liver injury cannot be ignored. Previous studies have shown that cirrhotic patients with relatively lower immunity are more susceptible to hepatic decompensation or acute chronic liver failure following influenza virus infection. Notably, similar results were also reported in a large, multicenter international cohort study; cirrhosis in COVID-19 patients was strongly associated with a poor model for end-stage liver disease scores and decompensated events. The authors show that mortality is strongly correlated with liver decompensation after SARS-CoV-2 infection; 63.2% of patients with a new decompensated event died, while the mortality rate in those without a new decompensation event was 26.2%.
According to a study by Sarin et al., decompensation of one fifth of cirrhosis was observed, in which 57% of patients developed liver damage and the mortality rate was 43%. Notably, in cirrhotic patients, the mortality rate from COVID-19 was significantly higher than in patients hospitalized due to bacterial infection. However, in a concurrently registered study conducted in the United States, Bajaj et al determined that mortality in patients with cirrhosis + COVID-19 was similar to that in patients with cirrhosis alone ( 30% vs 20%. , P = 0.16), but higher than in patients on COVID-19 alone (30% vs 13%, P = 0.03) after age/sex matching .
In this study, the Charlson Comorbidity Index, a comorbidity prognostic score was identified as the only independent variable predicting mortality in the entire matched cohort [odds ratio 1.23, 95% confidence interval (CI): 1.11-1.37; P < 0.001]. Therefore, whether the mortality rate in cirrhotic patients infected with SARS-CoV-2 is higher than in patients with other viral or bacterial infections remains to be determined.

2. Chronic hepatitis B patients co-infected with severe acute respiratory syndrome (SARS) virus are more likely to develop severe hepatitis
Based on previous studies, chronic hepatitis B patients co-infected with severe acute respiratory syndrome (SARS) virus are more likely to develop severe hepatitis. One reason may be that the SARS virus triggers massive HBV reactivation and replication, and that chronic hepatitis B patients co-infected with the SARS virus may need a longer time to completely clear the virus. SARS from their bodies. Very recently, an observation from China revealed that two patients with HBV infection had a slower clearance of SARS-CoV-2 (mean difference 10.6 days; 95% CI: 6.2-15.1). day).
Possible mechanism involves T-cell dysfunction in HBV-infected patients, which weakens the body's immune response to other viruses, but is there an exact link between the two? whether this virus or not is still to be elucidated. However, Chen et al. reviewed the clinical features of patients coinfected with SARS-CoV-2/HBV and found no significant difference in liver function index between 20 HBV-infected patients (6). ,1%) and 306 patients without HBV infection (93.9%). Furthermore, there is no evidence that SARS-CoV-2/HBV co-infection will reduce hospital discharge rates and prolong hospital stay.
A similar phenomenon was observed in another study that showed that patients with COVID-19 co-infection with hepatitis B were not significantly associated with worse outcomes than those without hepatitis B.
3. Patients with pre-existing NAFLD infection with SARS-CoV-2 are more likely to have abnormal liver function
Patients with non-alcoholic fatty liver disease (NAFLD) have previously been reported to be more susceptible to liver damage with SARS-CoV-2 infection. Many of these are cases of mild to moderate liver damage, and severe disease is rare. Ji et al showed that patients with pre-existing NAFLD infection with SARS-CoV-2 had a higher likelihood of liver function abnormalities during hospitalization, a higher risk of disease progression, and a higher duration of disease progression. Shedding of the virus longer than in people without NAFLD.
In this study, the liver injury model was predominantly hepatocellular rather than cholestatic, which is in contrast to the existing finding that SARS-CoV-2 has a high affinity for the expressed ACE2 receptor expressed in biliary cells. Metabolic diseases, such as obesity, hypertension, diabetes, and cardiovascular disease are common in patients with NAFLD. Studies have shown that coexisting metabolic risk factors in NAFLD patients are independent risk factors for severe COVID-19 disease, and the risk of severity increases with the number of factors. existing metabolic risk factors.
To further verify whether NAFLD itself affects liver function in COVID-19 patients, Hashemi et al adjusted for potential confounders (age, sex, hypertension, diabetes) diabetes, obesity, hyperlipidemia, heart disease, and lung disorders) and determined NAFLD was still independently associated with ICU admission (49.3% vs 35.0%, P = 0.028) and mechanical ventilation ( 47.8% vs 30.3%, P = 0.0055), but not related to mortality.
NAFLD patients infected with SARS-CoV-2 have higher rates of transaminase elevations on admission. Coincidentally, a very recent study revealed a similar finding that NAFLD was an independent predictor of liver damage in COVID-19, but not a predictor of mortality and severity. disease severity (manifestation or progression). However, the debate regarding whether NAFLD increases the risk of death in COVID-19 patients continues.

4. Liver transplant recipients are also a particular population affected by the global spread of COVID-19
Prolonged immunosuppressive therapy may increase the risk of respiratory viral infections, especially in patients with preoperative organ decompensation and chronic disease. A prospective cohort study of 111 cases found that liver transplant patients had an increased risk of SARS-CoV-2 due to chronic immunosuppression, but mortality was lower than mortality. in the general population. Mycophenolate, an initial immunosuppressive drug, was identified as an independent predictor of COVID-19 severity, but no such decline was observed with calcineurin inhibitors or everolimus.
In a case series in Brazil, a negative effect of COVID-19 on liver transplantation was reported, especially in elderly patients with comorbidities. One case was a 69-year-old patient with severe cardiovascular disease who presented with rapid deterioration after being diagnosed with COVID-19 and another case was a NAFLD patient with renal failure complications, who ultimately died. secondary bacterial infection. However, different opinions have been relayed in other studies. A large international observational study conducted by Webb et al showed that liver transplantation did not significantly increase ICU admission and mortality risk. Similarly, D'Antiga et al. also showed that patients with COVID-19 who received a liver transplant were not at increased risk for severe lung disease, despite their immunocompromised status. Furthermore, the three COVID-19-related deaths observed at a transplant center in Italy were patients on long-term therapy with minimal immunosuppressive regimens, not patients with completely immunosuppressed transplant recipient.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesCai Y, Ye LP, Song YQ, Mao XL, Wang L, Jiang YZ, Que WT, Li SW. Liver injury in COVID-19: Detection, pathogenesis, and treatment. World J Gastroenterol 2021; 27(22): 3022-3036 [DOI: 10.3748/wjg.v27.i22.3022]