This is an automatically translated article.
The article is written by Master, Doctor Mai Vien Phuong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
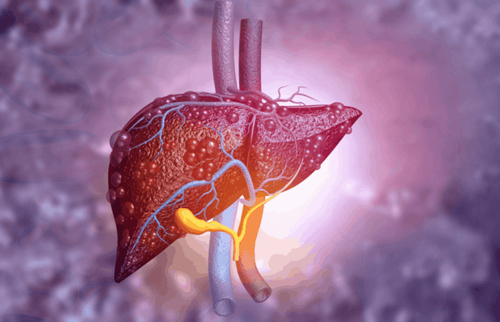
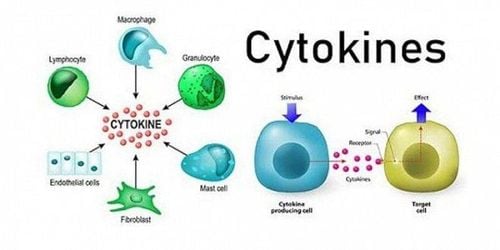
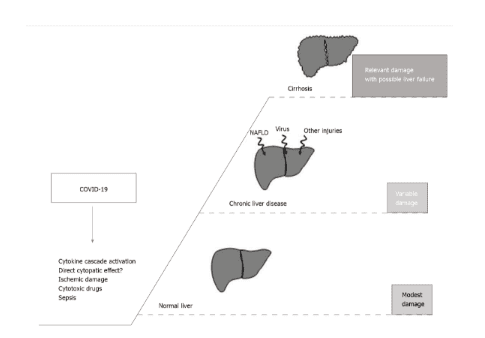
Currently, it is not entirely clear what causes liver failure during the covid-19 infection. However, covid-19 infection is characterized by significant activation of cytokine cascade, sepsis, and altered hepatic perfusion that can identify significant depletion of liver reserve in cirrhosis.
1. Reasons for liver failure in covid-19
The liver has a central role in the body's homeostasis, contributing to detoxification, catabolism, and the synthesis of important factors such as plasma proteins. ACE2 is significantly expressed only by cholangiocytes in the liver, however transaminases are elevated in more than one-third of hospitalized covid-19 patients.Currently, the reason for liver failure in the SARS-CoV-2 infection is not completely clear and many factors such as: direct impact of the virus, cytokine release, ischemic injury, drug use Hepatotoxicity, sepsis, and other factors may contribute to damage.
While covid-19 appears to cause only a transient change on examination in patients with normal liver function, it is worrisome, more severe sequelae are often observed in patients with reduced liver reserve. In addition, the risks of covid-19 in immunosuppressed patients (transplant or autoimmune liver diseases) are also described. Direct viral action, cytokine release, ischemic injury, hepatotoxic drug use, sepsis, and others may contribute to the damage.
2. Covid-19 in cirrhosis
Several factors can lead a patient with cirrhosis from a clinically compensated to a decompensated state. Among these, infection plays a related role in promoting the occurrence of acute-over-chronic liver failure (ACLF). In this view, SARS-CoV-2 infection is characterized by critical activation of cytokine cascade, sepsis, and altered hepatic perfusion, which may identify significant depletion of liver reserves in cirrhosis. .
Several studies evaluated the clinical outcome of covid-19 in cirrhotic patients. Preliminary data coming from two international registries and including 103 covid-19-positive cirrhosis patients show increased mortality relative to the general population. Furthermore, increased mortality is strongly related to the degree of pre-existing liver function impairment.
In the APCOLIS study, the worst covid-19 outcome in cirrhosis was again confirmed. 43 cirrhotic patients present:
Increased need for ICU care; More liver related complications; Increased mortality compared with CLD patients without cirrhosis. Covid-19 identifies the onset of decompensated cirrhosis or ACLF in one-fifth of cirrhotic patients. Child Pugh score >9 is a significant predictor of mortality.
3. What do the studies say?
A study conducted in Italy compared 30-day hospitalization mortality in a group of patients with covid-19 with or without cirrhosis. All-cause mortality was found to be significantly higher in cirrhotic patients. In addition, this study also demonstrated a decline in liver function in patients with long-standing stable liver disease.
In fact, worsening Child-Pugh scores have been observed, ranging from A score at admission to B/C status during hospital stay. The mortality rate caused by covid-19 in patients with decompensated cirrhosis has been increased compared with other infectious causes.
4. Patients with hepatocellular carcinoma with liver failure are classified as high-risk
Clearly, many patients with HCC have underlying liver failure that places them at higher risk, with clearly poor clinical outcomes. Considering this increased risk, the American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver (EASL) recommend prolonged clinical and ultrasound follow-up for patients with cirrhosis. liver, so as not to expose them to or spread in treatment sites, delay local HCC treatment if possible in patients with relatively stable disease, reserve interventions for patients who benefits outweigh the risks of SARS-CoV-2 infection.
However, a relationship between a decline in the immune system (for cancer, immune disease, or a transplant) and worse covid-19 outcomes has yet to be proven.
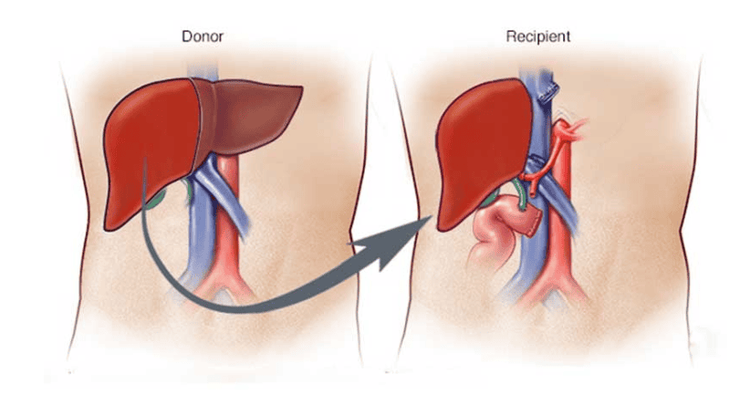
5. Covid-19 in liver transplant patients
As it is assumed that the integrity of the immune system is important to prevent the most severe sequelae of covid-19, since the beginning of the pandemic, concern has been heightened about the outcome. Possible outcomes in liver transplant (LT) patients on continuous immunosuppressive regimens. However, current data do not confirm this disturbing view.
An initial pediatric analysis from Northern Italy (an area hit hard by the pandemic) found that only three children were infected with covid-19 and with results that were not worrisome, in Some have a transplanted liver or are undergoing chemotherapy. Data on adult liver transplant recipients from the same geographic region showed different results. Three patients who received a liver transplant more than ten years ago and contracted COVID-19 died from complications. All were metabolically impaired (diabetes, hypertension) and >65 years old.
Paradoxically, their immunosuppressive regimen was less than that of patients with a shorter history of transplantation, suggesting that immunosuppression may be protective rather than detrimental. A series of studies have been published, collecting data from two international registries (COVID-Hep and SECURE-Cirrhosis). In this study, data from 151 liver transplant patients were compared with data from 627 control patients. The main factors associated with mortality in multivariate analysis were: Age, creatinine level and non-hepatic malignancy. Liver transplantation and immunosuppressive regimens were not associated with an increased risk of death. Finally, liver transplant patients required more frequent invasive ventilation (20% liver transplantation vs 5% controls; P < 0.001), while overall mortality was increased in non-transplant controls (19% liver transplantation). liver transplantation compared with 27% of controls; P = 0.05).
A prospective study in Spain re-evaluated this issue in 111 liver transplant patients with covid-19. Although mortality is slightly lower in liver transplant patients, the use of mycophenolate (particularly at doses > 1 g/day) is associated with an increased risk of severe covid-19 disease. From these findings, the authors suggest a possible benefit in reducing mycophenolate in covid-19 patients with liver transplantation, while complete discontinuation of the drug is not recommended. Taken together, the available data do not suggest an increase in mortality in liver transplant patients with covid-19, however enhanced surveillance would be the best option in these populations, as morbidity increases. as reported by several studies. Although a possible adverse effect on mycophenolate has been suggested, there is still a lack of clear research on the relationship between immunosuppression and the severity of covid-19.
6. Conclusion
The impact of covid-19 on liver health is complex and depends largely on the liver's basic functional reserve. It is currently unknown what causes elevated liver enzymes in a significant number of covid-19 patients. As a general rule, the effects of covid-19 are unlikely to be significant on normal livers, but concern persists for patients with impaired liver function. Expert associations, such as AASLD or EASL, are working hard to establish indications on issues such as liver transplantation and clinical management of patients with liver disease during the SARS-CoV-2 pandemic, also because lack of corroborating evidence.
While this scenario is rapidly evolving, there may also be some disturbing variations, other problems that are increasing for patients with liver disease. Among the pandemic-related and non-covid-19 side effects, the reduction of medical resources for liver disease patients can significantly affect their morbidity and mortality. An Italian study demonstrated that there was a 25% decrease in transplant activity associated with increased ICU saturation during the first 4 weeks of the national pandemic. Sudden interruption of HCC surveillance in the majority of cirrhotic patients will also affect the future.
Finally, a recent study that modeled a one-year delay in HCV cure, since the onset of the pandemic, estimated an increase of more than 100,000 deaths and liver-related cancers in population affected by this virus in the coming years.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Signorello A, Lenci I, Milana M, Grassi G, Baiocchi L. COVID-19 in normal, diseased and transplanted liver. World J Gastroenterol 2021; 27 (20): 2576-2585 [DOI: 10.3748 / wjg.v27.i20.2576]