This is an automatically translated article.
For many people with laryngeal or nasopharyngeal cancer, ending treatment with laryngeal surgery can be both stressful and exhausting. Some people who remain after surgery to remove a laryngeal tumor may still have regular treatment to control the cancer. So what will life be like after laryngectomy? Read on to learn how to live with cancer and after vocal cord surgery.
1. Laryngeal tumor removal surgery
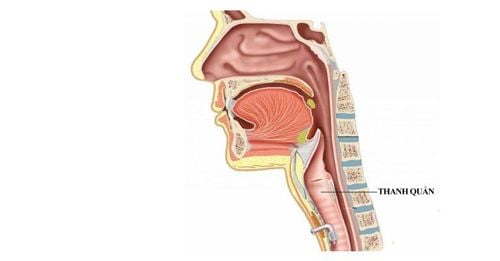
Laryngectomy is a surgery performed to remove the larynx. The specialist will perform this procedure. The larynx is the "voice box," or vocal cords, that vibrate as air passes through them during exhalation. This vibration produces sound, which is made into speech by parts of our mouth.
If the larynx is removed, a sound cannot be made when speaking. But only partial resection of the vocal cords can still allow the patient to speak, although in many cases speech will not be the same as it was before surgery and it can be more difficult for people to understand. In addition, the windpipe (breathing tube) is diverted when the larynx is removed, resulting in a hole in the neck that the larynx will breathe through. This is called "neck breathing".
Partial laryngectomy: When part of the larynx is removed. There may be a temporary tracheostomy that will be removed soon after. Partial surgery is only applied to cancer cases, mild lesions. Total laryngectomy: A tracheostomy will be performed to create a new way of breathing. This procedure may require removal of part of the pharynx (the tubular structure that connects the nose, larynx, and lungs), some lymph nodes, and some nearby muscles. The surgeon may perform a transesophageal aspiration (TEP), or place a hole in both the trachea and esophagus, for future laryngotracheal placement. Once the surgery is complete, your throat muscles and the skin on your neck will be stitched together with surgical stitches. The patient may have a drainage tube placed in the neck before being taken to the recovery room. The tubes will drain fluid and blood for a few days after the laryngectomy.
2. What is the mental impact after laryngectomy surgery?
2.1. Psychological impact. Laryngectomy is an important procedure in helping patients talk and breathe on their own. As a result, the patient may feel a loss of interest, anxiety or feel stressed, anxious leading to fatigue, depression after the procedure.
Some patients may be more affected than others. However, all patients may need the help and support of others, including friends and family, or professionals to feel better.
It is important to give yourself and those around you time to adjust to your life after laryngectomy.
Always think positive, always optimistic. When the sick person feels sad, worried, angry or distressed, remember that these are very common emotions. Try not to worry people too much.
So how do patients deal with the psychological effects of laryngectomy. Here are some effective solutions:
Find a new way of communicating that works best for the patient, as not all communication techniques after laryngectomy work for all patients . Expressing your feelings to a trusted friend or professional counselor can help you feel better. Talk to others, especially those who have also had laryngectomy, to get over the situation early. Try to change your diet to a healthy one. Find ways to help yourself relax, avoid fatigue. Get as much physical exercise as possible. 2.2. Concerns about safety after surgery. Wear a medical alert bracelet to determine if the patient is breathing normally with a breathing aid.
This is important when CPR, or oxygen delivered through the patient's mouth, is not effective. Or in case of need, you can ask for the support of nurses and doctors when they are not there.
Bring something that can be used as an alarm in an emergency when the sick person needs to scream for help. For example, a keychain or bell alarm can call attention to a sick person.
If the patient cannot speak or is too difficult to understand, bring paper and a pen to write so that can convey what the patient wants to say more easily.
Because the air you breathe does not pass through the nose, the patient's ability to smell will be reduced, which can cause safety problems such as: the patient may not be able to smell smoke from fire, gas. natural or spoiled sour food. Make sure the patient's room has a working smoke detector and change the batteries every 6 months.
2.3. Some issues that patients need to pay attention to after laryngectomy surgery Shower: After laryngectomy, patients need to avoid showering so that water does not enter the stoma.
Exposure to clean air: Remember that the air entering the vent when the patient breathes will go directly to the patient's lungs. Therefore, patients after laryngectomy should be careful with dust, pet hair, aerosols, etc. - And the patient should use an additional cover for the air outlet, to filter the air when exposed to a dusty environment.
Humidification: Before surgery, the air the patient breathes is humidified by the nose and mouth. After surgery, the patient is no longer able to properly humidify himself. Dry air leads to increased mucus production as the lungs try to humidify the air. The person will need to learn how to increase the humidity in the air when breathing and retain this moisture. Some ways to increase humidity are to use a cool mist humidifier when sleeping, or drop physiological saline.
3. Life after laryngectomy.
3.1. Restoration of voice after total laryngectomy. A total laryngectomy will remove your larynx (voice box) and you will not be able to speak with your vocal cords. After a laryngectomy, the patient's trachea (windpipe) is separated from the throat, so the patient cannot get air from the lungs out through the mouth to speak. But there are ways a person can learn to talk after a total laryngectomy:
Tracheoesophageal puncture (TEP): This is the most common way surgeons try to restore their voice. speak. It may be done during surgery to treat cancer or soon after. This procedure creates a connection between the trachea and the esophagus through a small opening at the stoma. A small one-way valve is placed in this hole so that the patient can push air from the lungs into the mouth. After this surgery, the patient can cover the stoma with a finger to push air out of the mouth, creating a sustained voice. It takes practice, but after surgery, you can study with a speech therapist to learn how to do this more easily and better.
Electrolaryngology: If the patient is unable to have TEP for medical reasons, or while the patient is learning how to use his or her TEP voice, an electrical device can be used to generate a mechanical voice. learn. The battery-operated device is placed in the corner of the mouth or on the skin of the patient's neck. When you press a button on the device, it will make a vibrating sound. By moving your mouth and tongue, you can form this sound into words. Patients will need training with a speech therapist to learn how to use it properly.
Esophageal speaking: With practice, some people learn to swallow air into the esophagus (the tube connecting the mouth to the stomach) and push it out through the mouth. As air passes through the throat, it causes vibrations that, with practice, can translate into speech. This is the most basic form of speech rehabilitation.
Learning to speak again will take a lot of time and effort, and the patient's voice will not be the same. Patients will need to see a speech therapist who is trained to help people who have had laryngectomy. The speech therapist will play an important role in helping the person learn to speak.
3.2. Support for swallowing problems and nutritional supplements after laryngectomy When treatments for laryngeal cancer or cancer of the lower pharynx can sometimes cause problems such as difficulty swallowing, dry mouth or even tooth loss. This can make it difficult for patients to eat and swallow, leading to weight loss and weakness due to poor nutrient absorption.
Some patients need to adjust their diet during and after treatment or may need additional nutrients. Some may even have to have a feeding tube inserted into the stomach.
Doctors and nutritionists need to support patients to help them maintain their weight and get the nutrients they need. Patients after laryngectomy also need to talk with the specialist about swallowing exercises and helping the patient to regain the ability to eat more normally after treatment.
3.3. Restoring the sense of smell Nearly everyone who has had laryngectomy will find that they can't smell things the same way they used to.
This is because air is no longer moving through the patient's nose. If the patient has lost their sense of smell, restoring the sense of smell can be another part of the patient's recovery. Problems with the sense of smell (called olfaction disorders) can affect a patient's appetite, sense of smell, ability to enjoy food, and food intake.
With olfactory rehabilitation, the patient can be taught techniques that induce nasal airflow and can help you restore your sense of smell. Examples include nasal airflow stimulation (NAIM) and polite yawning. Olfactory rehabilitation (rehabilitation) is available at some major medical centers.
4. What to do to reduce the risk of laryngeal cancer, oropharyngeal cancer after laryngectomy?
Quit smoking: Patients who smoke during cancer treatment will be the cause of reducing the benefits of treatment, increasing the risk of cancer recurrence. Smoking also increases the risk of new cancers. Laryngeal and oropharyngeal cancer survivors who continue to smoke are more likely to die of cancer. Quitting smoking (before, after treatment, if possible) is the best way to improve patient survival.
Adopt healthy behaviors: Patients after laryngectomy need to maintain healthy behaviors such as a nutritious diet, regular exercise and sports, and keeping a healthy weight. reasonable to maintain good health for the patient. Those good activities can have more positive effects on the patient's health.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: thancguide.org, ancer.org, oncolink.org