This is an automatically translated article.
Posted by Doctor Do Van Manh - Emergency Resuscitation Department - Vinmec Ha Long International General Hospital.For patients with severe acute respiratory failure unresponsive to mechanical ventilation support and patients with acute heart failure such as acute viral myocarditis that does not improve with conventional treatments, the birth of the ECMO method applied by emergency physicians.
1. What is the exchange of oxygen across the outer membrane of the body?
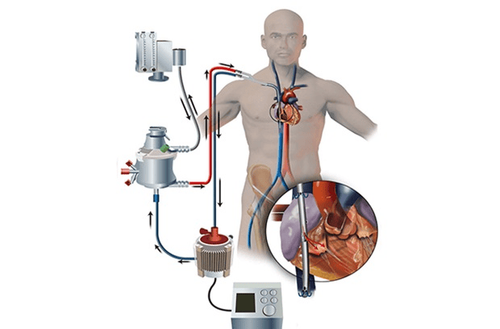
Extracorporeal membrane oxygenation (ECMO) is a method of respiratory and circulatory emergency when the heart or lungs or both cannot function properly. This technology (ECMO) can replace the heart or lungs or both in a short time. Blood is taken out of the body from the veins through a filter that functions like a human lung, the filter will bind the blood with oxygen before returning it to the vein to enter the body. Similarly, blood is taken from a vein through a membrane system and returned to an artery for cases requiring circulatory support (cardiac support).2. In what cases is ECMO used?
The purpose of ECMO technique is to ensure that the patient's body has enough oxygen. Although ECMO does not cure heart or lung disease, it helps patients overcome the critical, combined with treating the cause and waiting for the recovery time, can reduce heart-supportive drugs, reduce ventilator support to reduce risk of injury from the ventilator.
Kỹ thuật ECMO giúp cứu sống nhiều trẻ nhỏ mắc vấn đề về sức khoẻ
Children are mainly applied, but in case of adults with heart failure, respiratory failure, it can still be used as usual. ECMO sends blood outside the body, then removes carbon dioxide and adds oxygen to red blood cells. This technology is applied to treat patients with end-stage disease, heart failure or severe respiratory failure. ECMO is also used to prolong life so that doctors can find the cause of cardiac arrest. In addition, the following conditions may be considered for the use of ECMO:
Respiratory failure if the ratio of arterial oxygen tension to inspiratory oxygen (PaO2 / FiO2) is less than 100 mmHg even though the machine breathing has been used at full capacity.
Respiratory failure due to abnormally high levels of carbon dioxide with an arterial pH less than 7.20
Cardiogenic shock
● Heart problems after heart surgery
● Cardiac arrest
Used to maintain health living during a heart transplant or placing a ventricular assist device or a lung transplant
Although controversial, ECMO treatment for septic shock is still being studied
Hypothermia with temperatures ranging from 24-28 °C and cardiac instability or with a temperature <24°C.
3. What ECMO methods are there?
There are two most common types of ECMO, venous-arterial ECMO and venous-venous ECMO, both of which work on the principle that blood is taken from the venous system outside the body, then oxygen is added and returned. about body. In venous-arterial ECMO the blood is returned to the arterial system and in venous-venous ECMO the blood is returned to the veins. However, venous-intravenous ECMO only supports respiration, not the heart.
Venous-arterial : This method is to place an intravenous catheter into the left or right femoral vein to draw blood out and an arterial catheter into the left or right femoral artery to return blood. blood into the body. The position of the right femoral vein catheter tip was kept immediately near the junction of the inferior vena cava and the right atrium while the tip of the right femoral artery catheter was in the iliac artery. In adults, access to the femoral artery is preferred because insertion is simpler than in young children
Phương pháp ECMO tĩnh mạch-động mạch
● Vein-venous: In this method, a catheter is placed into the femoral vein to bring blood out and the right internal jugular vein to return blood. In addition, a double-ended catheter is inserted into the superior and inferior vena cava to drain blood and return it to the right atrium after the addition of oxygen.
4. What complications are common with ECMO treatment?
Neurological
Common consequences in adults treated with ECMO are neurological injury including subarachnoid hemorrhage, infarction, ischemia in sensitive areas of the brain, cerebral hypoxia, unexplained coma and brain death. The probability of bleeding is 30-40% due to the continuous infusion of heparin-containing anticoagulants causing platelet dysfunction. Correction of surgery is to maintain a platelet count greater than 100000/mm3.
● Blood:
Blood platelets will be reduced due to anticoagulant heparin, to overcome, use anticoagulant without heparin. There is also a retrograde blood flow in the aorta and downward even when the femoral artery and vein are connected to the ECMO machine. If the tube position of the catheter tip is not maintained in the original position, blood stasis can occur which can cause blood clots.
● Premature birth:
If the baby is less than 32 weeks old, ECMO will not be used to maintain life because the risk of intracranial hemorrhage is very high.

Điều trị bằng phương pháp ECMO cũng có thể xảy ra một số biến chứng nhất định
5. What should doctors pay attention to when using ECMO?
● VV ECMO is commonly used for respiratory failure and VA ECMO is used for heart failure.
● In VV ECMO, the higher the blood rate, the better because it supports the exchange of oxygen. But conversely, in VA ECMO the blood rate must be high enough to have adequate venous pressure and oxyhemoglobin saturation (measured on drained blood) but low enough to warrant delivery.
● If the patient is fluid overloaded, aggressive diuretic therapy should be instituted until stable on ECMO. In contrast, ultrafiltration can be easily performed while the patient is being kept alive by ECMO.
● Blood clots can form when blood exits the left ventricle due to impaired left ventricular function.
● After the patient is stabilized, it is necessary to measure the oxygen saturation in the blood drawn from the vein.
6. What are the risks of using ECMO machines?
Doctors taking care of patients use ECMO machines to avoid any possible complications for the patient. Some serious problems that can occur when a patient uses an ECMO machine include:
● Hemorrhage : Bleeding in different parts of the body due to the anticoagulants the patient needs to take while on the ECMO machine. . Most dangerous when bleeding occurs in the brain, lungs, catheter sites or stomach bleeding.
Các vị trí đặt ống thông có nguy cơ gây xuất huyết cho bệnh nhân
● Renal failure : Patients using ECMO machines sometimes do not receive an adequate blood supply to the kidneys. This can cause the kidneys to stop working and is called "acute renal failure". If the kidneys stop working, the patient may need dialysis, also known as dialysis. Damaged kidneys can be restored. However, in some cases, patients may need lifelong dialysis.
● Infection : The catheters of the ECMO machine pass directly from the outside of the body into the patient's blood stream. This increases the risk of infection, because these catheters are the entry point into the body for pathogens. The infection can reach the lungs, or any other organ of the body. Infections in ECMO patients can often be treated with antibiotics. However, some patients develop concurrent infections while using the ECMO machine, which can result in worsening illness and organ damage.
Leg Injury: Some patients are connected to the ECMO machine through a vein or artery in their thigh. In some cases, this can reduce blood flow down that leg, and tissue in the leg can die. If this happens, doctors will try to restore blood flow to the leg. This often means changing the catheter site to another part of the body. However, sometimes the leg damage is so severe that the patient needs surgery and possibly amputation.
● Stroke : In patients who are on an ECMO machine, certain areas of the brain may not get enough blood flow because of small blood clots. This can cause a stroke, and an area of the brain can be permanently damaged. The damaged brain area will show the corresponding stroke symptoms. Some patients will not be able to move certain parts of their body or be unable to see, remember, talk, read or write. Sometimes some people can recover some function after a stroke, but this is very rare. Fortunately, stroke is very rare and <5% of the time patients use the ECMO machine.
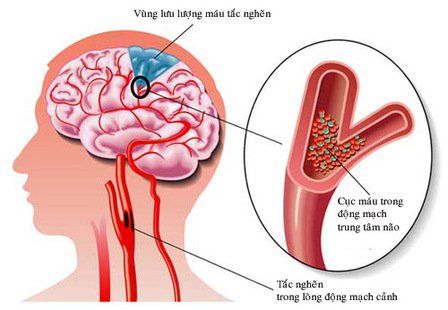
Cục huyết khối nhỏ gây cản trở lưu thông máu đến một số vùng não của bệnh nhân
7. How to monitor a patient using an ECMO machine?
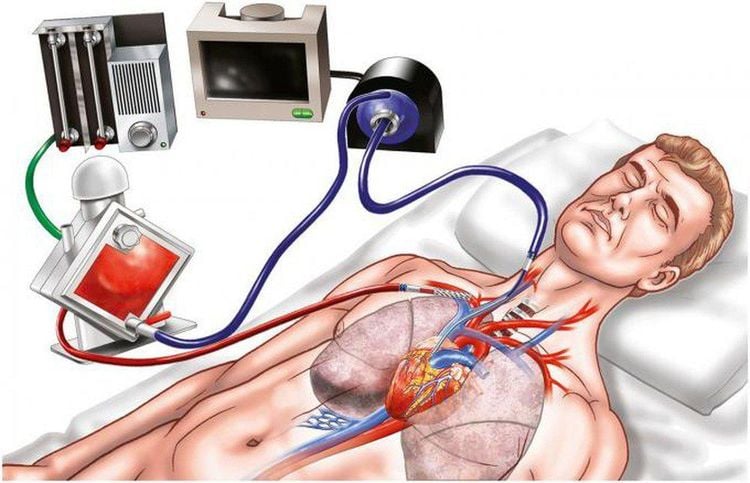
The ECMO machine is connected to the patient through plastic tubes (cannula tubes). These tubes are placed into large veins in the legs, neck, or chest. The ECMO machine pumps blood from the patient's body to an artificial lung (oxygenator) to replenish O2 and remove CO2 from the blood.
So it will replace the patient's lung function. The ECMO machine will then pump blood back to the patient with a pumping force equal to the work of the heart's contraction, which replaces the heart's function. The ECMO machine is operated by an ECMO specialist, or a nurse or respiratory therapist with extensive training in ECMO. Specialists will adjust the settings on the machine to ensure that it is providing patients with the full heart and lung function they need.
Any patient on the ECMO machine in the ICU is being monitored with a monitor. Monitor will measure heart rate, blood pressure, and blood oxygen saturation. Patients using ECMO machines should have their blood drawn regularly for O2 and CO2 levels. These tests are called arterial blood gases. These patients also need anticoagulants to prevent blood clots. Therefore, the blood also needs to be checked regularly to make sure that the blood is not clotting. Doctors will use all of these results to see how well the ECMO machine is supporting their patients and make adjustments if necessary.
The ECMO machine can help save a patient's life, but it does not treat the patient's illness or injury. The ECMO machine simply provides support to the patient while doctors treat the patient's underlying medical condition or injury (such as an infection) or while waiting for the transplant organ to be ready. Doctors always try to help patients wean from ECMO as soon as possible. Some medical conditions or injuries can be treated quickly, and these patients only need to use the ECMO machine for a few hours. In other cases where long-term treatment is required to be effective, the patient may be able to use the ECMO machine for a few days to a few weeks. Unfortunately, in some cases, patients do not improve enough to wean ECMO. ECMO cannot save all patients' lives, but it can improve survival for critically ill patients who do not respond to other supportive treatments.
Bệnh nhân được kết nối với hệ thống máy ECMO tại Bệnh viện Vinmec
Patients connected to an ECMO machine for the first time are usually sedated so they won't feel the catheter entering their arterioles. A patient on an ECMO machine usually has been previously ventilated with an endotracheal tube placed through the mouth or nose into the trachea.
Once connected to the ECMO machine, the catheters should be painless. Patients who are on an ECMO machine may be given medication (sedation or pain reliever) to help them feel comfortable. These drugs can also make them drowsy. Other patients can be awake, talking, and interacting with people while they are using the ECMO machine. In some cases, patients can exercise to help recover while using the ECMO machine. However, some movements can cause the ECMO tubes to bend, so patients need careful support and supervision while they are exercising.
Invasive mechanical ventilation is performed at Vinmec Ha Long International Hospital with patients with acute respiratory failure. The hospital uses a highly configurable ICU ventilator system for adults, children and infants.
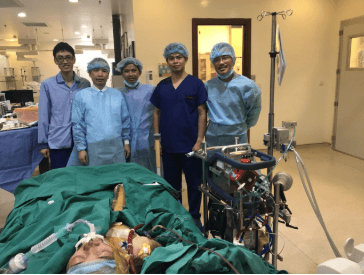
Especially, the team of doctors performing the technique are all doctors from the Emergency Department with high professional experience:
● Ths.BS.Nguyen Nam Duong
● Specialist I Doctor Do Van Manh
● MSc Vu Manh Thang
Customers can go directly to Vinmec Ha Long to visit or contact hotline 0203 3828 188 for support.