This is an automatically translated article.
The article was written by Master, Doctor Mai Xuan Thien - Emergency Department, Vinmec Times City International General Hospital.Anaphylaxis rarely presents as an acute coronary syndrome with or without pre-existing coronary artery disease. The diversity of the underlying disease makes up the diversity in the clinical presentation of this acute coronary syndrome.
The following article presents 3 clinical cases of acute coronary syndrome associated with anaphylaxis representing different clinical manifestations of this phenomenon. The main pathophysiological mechanism for this syndrome is the release of chemical mediators during the hypersensitivity response to food, insect stings, or drugs. It is important to recognize Kounis syndrome in patients exposed to an allergen.
1. Allergic-associated acute coronary syndrome
Acute coronary syndromes associated with mast cell activation due to anaphylaxis, hypersensitivity or allergic reactions were first described by Kounis and Zavras in 1991 as “allergic angina pectoris allergic reaction” or “allergic myocardial infarction”.The pathogenesis of Kounis syndrome involves the release of cytokines through the activation of mast cells, leading to coronary vasospasm or destabilization or rupture of atherosclerotic plaques of the coronary arteries. Kounis syndrome has been described in a variety of conditions including exposure to environmental factors or drugs.
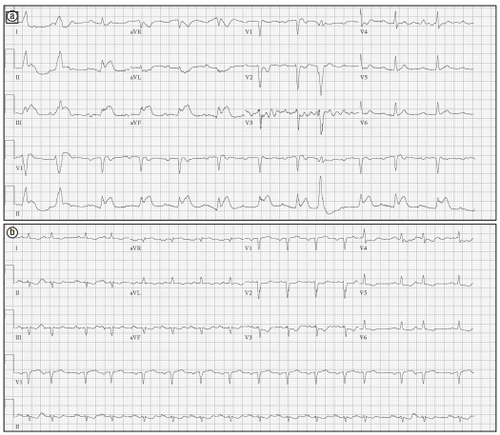
Recently, manifestations of post-allergic angina are more commonly described. In the following clinical cases we describe three different clinical cases of ST-segment elevation following anaphylaxis, including ST-segment elevation myocardial infarction with or without pathology. previous coronary artery (coronary vasospasm).
2. Description of clinical cases of acute coronary syndrome
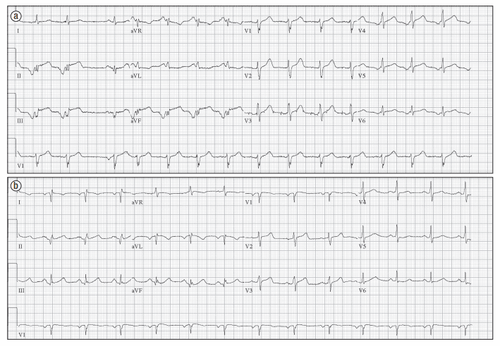
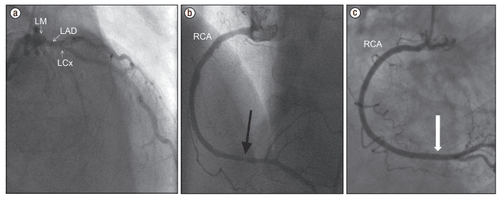
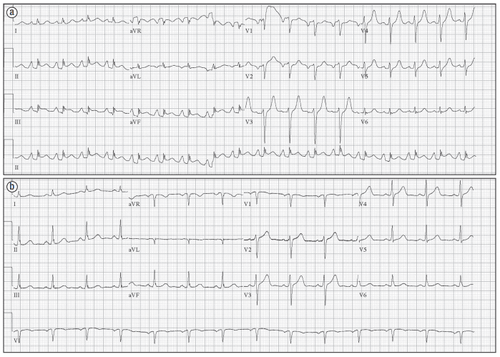
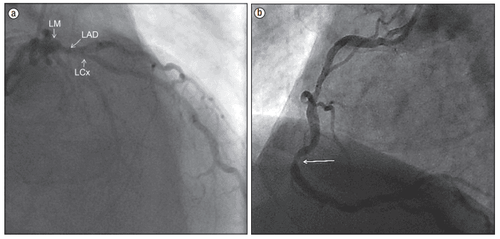
A 64-year-old male patient has a history of peripheral arterial disease, chronic obstructive pulmonary disease, coronary artery disease, dyslipidemia and hypertension. Admitted to the hospital with itching, chest pain, shortness of breath, and vomiting shortly after having dinner at a pea salad restaurant. Electrocardiogram on admission showed ST elevation in leads II, III, and aVF (Figure 1a). The patient has a history of allergy to peas and peanuts. Vital signs on admission are temperature: 37oC, Blood pressure: 81/60 mmHg, Breathing rate: 20 times/minute, Pulse 91 times/minute. Physical examination revealed laryngeal stridor, generalized erythema, and weak peripheral pulse. Blood tests showed white blood cells 19.5 G/l, CK and Troponin I all showed normal results.Emergency coronary angiography showed moderate stenosis of the proximal and middle segments of the anterior septal artery and the right coronary artery, which improved with nitroglycerine (Figure 2). The definitive diagnosis was coronary vasospasm secondary to an anaphylactic reaction to peas. Treatment initiated with intravenous hydrocortisone, diphenhydramine, and famotidine resulted in clinical improvement. The patient's blood pressure improved by 120/60 mmHg. Repeat electrocardiography showed normal results (Figure 1b). Patient is discharged.
3. Discussion
The three types of Kounis syndrome are described through three clinical schools. Type I includes patients with normal coronary arteries without risk factors for coronary artery disease, allergic conditions leading to coronary vasospasm, cardiac enzyme indices for diagnosis of myocardial infarction, and positive results. normal fruit. This variant represents endovascular dysfunction or microvascular angina. Type II includes cases with coronary artery damage but coronary artery disease in inactive form, in cases of allergy can cause the plaque to become unstable and rupture, leading to myocardial infarction. Cardiac arrhythmia or coronary spasm with normal cardiac enzymes. Type III includes coronary stent occlusion secondary to an allergic reaction. Allergic reaction anemia is a condition secondary to the release of chemical mediators including histamine, tryptase, chymase, platelet-activating factor, cytokines, and prostaglandins, and leukotriene synthesis leading to spasm. coronary artery. Vigorito et al. have previously described paradoxical vasoconstriction mediated by the histamine-1 receptor. Many cases of Kounis syndrome have also been described in the literature before.The clinical cases we describe are Kounis syndrome as a completely different phenomenon from the usual cases of anaphylaxis or allergies. Some authors have suggested that the vasospasm process is dominant to explain the pathogenesis of the syndrome. The classic theory of anaphylaxis is formerly known to be vasodilatation and reduced venous return to the heart, increasing vascular permeability and leading to decreased cardiac output, resulting in decreased coronary perfusion and injury. heart muscle. Therefore, distinguishing primary myocardial injury secondary to mast cell activation from myocardial hypoperfusion can be challenging and an alternative hypothesis for acute allergic coronary syndromes (presentation of ST elevation). It is important to recognize these forms of Kounis syndrome providing the basis for appropriate treatment and care. The diagnosis of true Kounis syndrome remains a challenge, requiring consideration of both co-occurring cardiovascular disease and anaphylaxis.
Treatment of Kounis syndrome requires the use of a number of common medications that must be carefully considered. Morphine and some other important medications for angina can aggravate anaphylaxis, as it can stimulate the release of histamine. Beta-blockers may also increase coronary vasoconstriction if used in Kounis syndrome because they do not antagonize alpha adrenergic activity. Epinephrine, the drug commonly used in anaphylaxis, should be used carefully with close monitoring, as it can aggravate coronary vasospasm and increase coronary ischemia in Kounis syndrome. The primary treatment of Kounis syndrome should focus on the allergic reaction and the removal of the allergen.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.