This is an automatically translated article.
The article was professionally consulted with Master, Doctor Do Xuan Chien - Head of Department of Medical Examination & Internal Medicine - Vinmec Ha Long International General Hospital.Ketosis in patients with diabetes is one of the serious complications of diabetes, which can be life-threatening. Therefore, diabetics need to pay attention to the signs of ketoacidosis in order to promptly detect and treat, avoiding the risk of dangerous complications.
1. What is ketoacidosis?
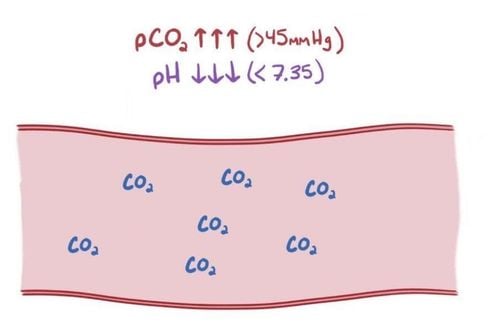
Diabetic ketoacidosis is a serious complication of diabetes that occurs when a person's body produces too much acid in the blood (called ketones). This condition occurs when the patient's body does not produce enough insulin, causing severe disturbances in the metabolism of proteins, lipids and carbohydrates.
Diabetic ketoacidosis includes 2 dangerous biochemical disorders: hyperglycemia, ketosis, acidosis accompanied by electrolyte disturbances. This is a medical emergency that needs to be monitored in the intensive care unit because of the risk of serious complications such as coma, cerebral edema, and even death.
2. Symptoms of ketoacidosis in patients with diabetes
Fatigue, blurred vision, hazy consciousness; Nausea, vomiting, abdominal pain; Excessive thirst, drinking a lot and urinating a lot; Weight loss; Blood glucose > 13.9 mmol/L (> 250 mg/dL) when measured with a personal blood glucose meter; Tachycardia, low blood pressure; Signs of dehydration: Dry lips, dry tongue, severe dry skin; Breathing has 4 stages: Inhale - stop breathing - exhale - stop breathing, the breath smells of ketones (smells of ripe apples). The smell of ketones occurs due to the elimination of the acetone-derived product from acetoacetate through the lungs; Body temperature often drops slightly due to varicose veins on the skin. This is a manifestation of a poor prognosis. Patients should call 911 immediately if they experience the following:
Blood sugar levels consistently higher than 300 mg/dL or 16.7 mmol/L; There are ketones in the urine, which cannot be reduced to the allowable limit; More than 1 symptom of diabetic ketoacidosis.

3. Causes of diabetic ketoacidosis
Insulin deficiency: Due to diabetes, stopping insulin treatment, incorrect insulin injection technique; Acute illness, infection (pneumonia, meningitis, gastrointestinal infection, urinary tract infection, acute pancreatitis, flu), trauma or surgery,... stimulates the body to produce a some hormones such as: Catecholamine, Cortisol and Glucagon, affect the action of insulin and cause complications of ketoacidosis; Physical and mental disorders; Heart attack, myocardial infarction, stroke ; Using hypoglycemic drugs improperly; Effects of alcohol use or drug abuse; Side effects of taking medications such as corticosteroids and some diuretics; Effects of endocrine diseases: hyperthyroidism, hyperadrenocorticism, adrenal myeloma; Stress.
4. Diagnosing ketoacidosis in diabetic patients
Clinical examination; Blood tests to measure ketone levels, glucose levels, and blood acids; Electrolytes ; Total urinalysis ; X-ray; Electrocardiogram: Measures the electrical activity of the heart. Note: It is necessary to differentiate the symptoms of hypotension, psychosis, and severe abdominal pain in patients with diabetic ketoacidosis from other conditions.
5. Treatment of ketoacidosis in patients with diabetes
Treatment of diabetic ketoacidosis mainly includes: prevention of dehydration, adequate insulin replacement, restoration of electrolyte balance and treatment of acid-base disorders. Specifically:
Make a treatment monitoring table: To monitor, list vital signs and plan to do laboratory diagnostic tests related to treatment procedures.
Insulin replacement: Use only rapid-acting insulin (regular insulin) to treat severe cases of ketoacidosis and should be used immediately after confirming the diagnosis. Rapid-acting insulin can be given at doses as high as 0.1 units/kg intravenously as a whole, followed by 0.1 units/kg/hour as a continuous infusion or hourly intramuscularly. This helps to replace insulin deficiency in diabetics.
When the patient is awake, starting to eat by mouth, can switch from intravenous insulin to subcutaneous insulin, the dose of insulin depends on the glucose level in the blood.
Fluid and electrolyte replacement: In most patients with diabetic ketoacidosis, the fluid deficit is 4-5 liters and needs to be replenished. Initially, 0.9% saline solution was chosen to supplement the patient immediately after confirming the diagnosis to re-dilate the constricted lumen. During the first hour, infuse at least 1 liter of 0.9% saline solution. Then, the amount of fluid should be infused at a rate of 300 - 500 ml/hour, combined with careful monitoring of the patient's serum potassium.
If blood glucose is above 500mg/dL, 0.45% saline should be used after the first hour. When blood glucose falls to 250 mg/dL or less, a 5% glucose solution should be used to maintain blood glucose between 200 and 300 mg/dL while insulin therapy is continued to remove ketones.
Note, it is necessary to make sure to supplement the necessary amount of fluid. If the supplement is not enough (at least 3 - 4L/8 hours) it will affect the patient's ability to recover; Excessive fluid intake (over 5L/hour) can lead to respiratory distress syndrome or cerebral edema;
Potassium replacement: Hypokalemia occurs in 5% of patients with diabetic ketoacidosis, potassium loss is mainly due to polyuria and vomiting. The patient has a deficiency of 3 - 6 mmol/kg, even up to 10 mmol/kg.
When serum potassium is < 5.5 mmol/l and the patient is not anuria, potassium should be started immediately from the start of treatment. With serum potassium in the range of 4 - 5 mmol/l, the starting potassium intake is 15 - 20 mmol/h (1g KCl/h), the potassium dose can be increased to 30 or 40 mmol/h (2g KCl/h). in the case of patients with hypokalemia from the outset.
On average, the amount of potassium needed in the first 24 hours ranges from 10 -30 g KCl. When recovered, can eat and drink, the patient can be prescribed to use potassium-rich foods such as tomato juice, grapes, bananas,...
Phosphate supplement: Rarely need supplement Phosphate in the treatment of diabetic ketoacidosis. However, if severe hypophosphatemia below 0.35 mmol/L (<1 mg/dL) occurs during insulin therapy, small amounts of phosphate should be rehydrated with phosphate salts.
Treatment of infections associated with: Indication to use antibiotics.

6. Prevention of diabetic ketoacidosis
Control diabetes by maintaining a healthy diet, daily physical activity, and taking medications as prescribed by your doctor; Patients need to know how to self-monitor blood glucose and urine ketones, control blood sugar and ketones if sick or stressed; When there is severe ketonuria and the urine glucose persists through many tests, the patient should supplement with insulin and liquid foods such as tomato juice, low-salt meat broth to replenish fluids and electrolytes for the body; Patients should contact their doctor if they have another medical condition, have persistent ketones in the urine, fever, abdominal pain, diarrhea, high blood glucose levels, persistent ketones in the urine, especially vomiting. vomiting or if the infusion rate has been adjusted with an insulin pump but there is no improvement in hyperglycemia and ketosis; Patients should not arbitrarily reduce the dose of insulin injection or voluntarily quit even in the case of another disease. Diabetic ketoacidosis is a dangerous complication that can lead to coma or death. Therefore, people with diabetes need to actively prevent this complication. At the same time, when there are warning signs of ketoacidosis, the patient should immediately go to the doctor for a definitive diagnosis and timely and effective treatment.
Periodic health check is one of the ways of early recognition and prevention of disease, especially for patients with signs of diabetes, from which to have a treatment plan with optimal results. Currently, Vinmec International General Hospital has general health checkup packages suitable for each age, gender and individual needs of customers with a reasonable price policy, including:
Health checkup package general Vip Special general health checkup package Standard general health checkup package Patient's examination results will be returned to your home. After receiving the results of the general health examination, if you detect diseases that require intensive examination and treatment, you can use services from other specialties at the Hospital with quality treatment and services. outstanding customer service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.