This is an automatically translated article.
The article was professionally consulted by resident Doctor Ho Thi Hong Tho - Neonatologist - Department of Pediatrics - Neonatology - Vinmec Phu Quoc International General Hospital.Jaundice due to increased free bilirubin in neonates is a physiological phenomenon. However, when the level of jaundice increases rapidly and is often quite serious and can cause brain damage, then cerebral palsy, severe sequelae if not actively treated. Blood type incompatibility between mother and child is one of the causes of severe neonatal jaundice.
1. What is blood group?
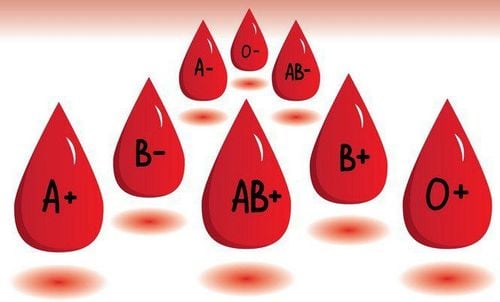
Blood type is one of the characteristics that identifies a particular person. Blood type is determined based on the presence of antigenic proteins on the surface of red blood cells.Based on the proteins on the surface of red blood cells, blood is classified into groups with the characters A, B, and O. Accordingly, the way to determine blood group according to ABO can be blood group A, blood group. B, blood group AB or blood group O. This is because there are two antigenic proteins, represented by A and B. A person with blood type A means that they have the A antigen on their red blood cells. The same goes for B antigens. However, a person with blood type AB means that both types of antigens are present on the blood cells while blood group O means neither antigens are present.
For the Rhesus (Rh) antigen system, blood will be classified into two groups with Rh positive or negative, written as Rh + or Rh-. People with blood group Rh being positive means having Rh protein on the surface of red blood cells and vice versa for Rh negative.
Thus, with only ABO and Rh blood group identification, when described together, there are eight different blood groups: A +, A-, B +, B-, AB +, AB-, O + and O-. However, this is just a common method of identification and there are many other ways to identify blood groups, but the popularity is low, so it is rarely mentioned.
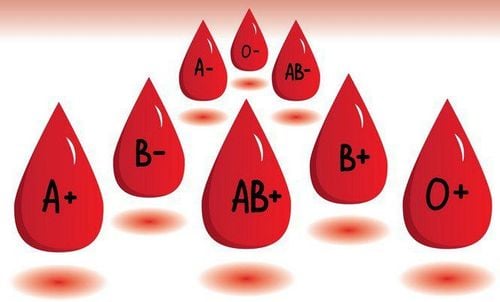
Nhóm máu gồm nhóm máu A, nhóm máu B, nhóm máu AB, nhóm máu O
2. What is blood group incompatibility?
The blood group of the fetus is determined by the combination of two sets of chromosomes from the egg and sperm. Accordingly, the child receives half of the genome from the mother and half of the genome from the father, that combination will determine which ABO and Rh blood groups the child belongs to.However, in some rare cases, blood group incompatibility still occurs between mother and fetus. This disagreement will be classified according to the blood group classification system.
2.1. Rh incompatibility
Rh incompatibility occurs during pregnancy if the mother is Rh- and the baby is Rh+. This is a serious problem when the mother's body does not recognize the Rh protein before and will treat it as a foreign substance (antigen). During pregnancy if the placenta is damaged (threatened of miscarriage) or when the placenta is aborted during labor, Rh antigens from the fetus enter the mother's circulation through the umbilical cord, the immune system will produce antibodies that attach to the antigen and launch an attack on the fetal red blood cells. As a result, it often causes miscarriage very early.Fortunately, however, this is not a common problem as most people have Rh+ blood type. Despite this, about 13% of women in the population are Rh- and are at risk of Rh incompatible pregnancies. This happens when the father is Rh+ or has no prior Rh status at all. Finally, Rh incompatibility between mother and fetus can cause a condition called hemolytic disease of the newborn. If the baby is still alive until birth, it will also have very severe neonatal jaundice.
2.2. Not compatible with ABO
The mother and fetus can also have ABO blood type incompatibility and can also cause hemolytic anemia in the newborn. However, compared with the Rh system, this incompatibility usually has less serious consequences. This is a condition that occurs when a mother has blood type O and the baby is A, B or AB. Like Rh incompatibility, this will trigger the mother's immune system to view the A or B antigens in the fetal blood as foreign substances and trigger an immune response, attacking and destroying them. .3. What is ABO incompatibility jaundice and hemolytic disease of the newborn?
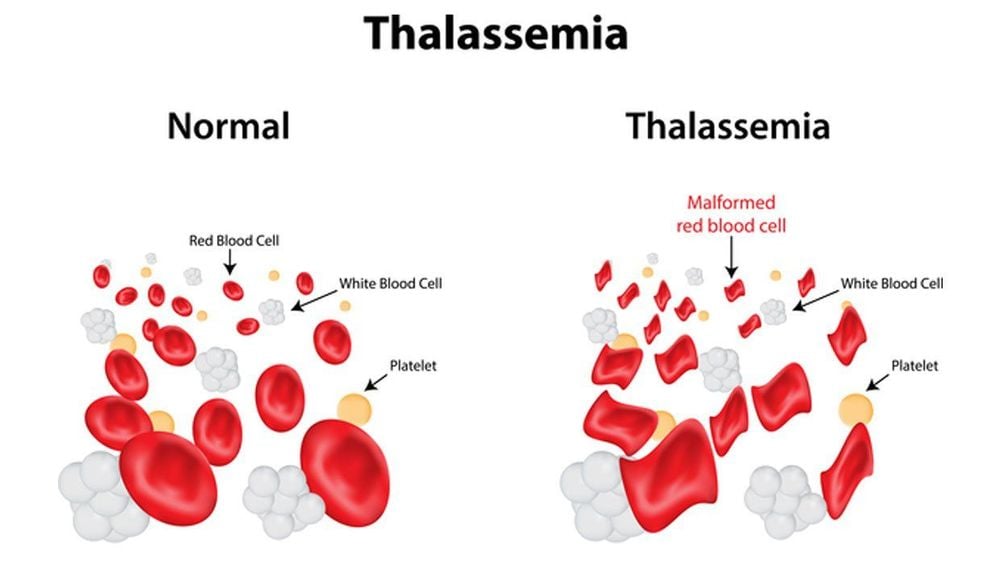
The blood incompatibility between the mother and the baby can cause various complications, the most prominent of which is hemolytic disease in the newborn with manifestations including anemia and jaundice. Jaundice has always been the most common symptom of hemolytic disease in neonates as jaundice occurs very early in the first 24 hours of life and progresses rapidly. As for the ABO blood type incompatibility, the severity is usually mild and will go away with time.However, with Rh incompatibility, the consequences can be very serious, sometimes life-threatening to the baby. At this point, babies can be born with severe jaundice, which is characterized by a build-up of a substance called bilirubin, which is released after the breakdown of red blood cells. It is the accumulation of bilirubin that is responsible for the characteristic yellow color observed in the skin and sclera of the eyes of children.
Normally, the liver will be the organ responsible for processing bilirubin and eliminating it from the body through the intestines and excretion. In children with congenital hemolytic disease, due to the massive breakdown of red blood cells taking place in too large numbers, the liver's metabolic rate cannot keep up, causing bilirubin to accumulate in the blood with high concentrations and expression. present jaundice.
Jaundice with increased free bilirubin is a normal physiological phenomenon after birth, it usually occurs on the 3rd to 5th day, lasts 7 to 10 days after birth. However, when there is a lot of jaundice, there can be serious consequences, such as accumulation of bilirubin, which can cause brain damage, called kernicterus.
Nuclear jaundice occurs when bilirubin levels are so high that it moves into the brain. At this time, the infant not only has severe jaundice but also may have signs of cognitive disturbances such as lethargy or lethargy, somnolence, and lethargy. In addition, the child also has other signs of brain damage such as muscle weakness, decreased reflexes alternating with muscle stiffness, back and neck arching, high-pitched crying, fever, and convulsions.
Maternal blood group incompatibility and nuclear jaundice are considered a medical emergency. Children need to be actively treated for bilirubin excretion with light therapy and considered in combination with a blood transfusion to minimize the amount of damage caused to the brain, to prevent progression to cerebral palsy due to jaundice.
Không tương thích ABO có thể gây ra bệnh tan máu bẩm sinh
4. How to prevent and treat jaundice caused by blood group incompatibility in newborns?
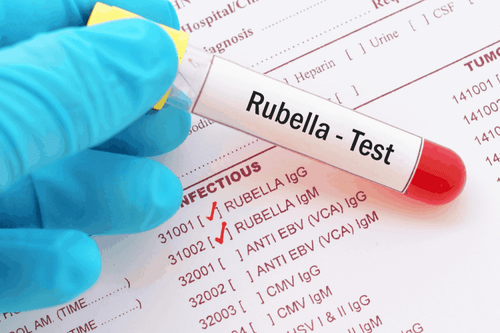
Fortunately, blood type incompatibilities can be proactively prevented with blood testing early in pregnancy. If an ABO or Rh blood type incompatibility is found, immunoglobulin therapy will be given for about 28 weeks of pregnancy. These proteins, when introduced into the mother's body, will neutralize the created antibodies as well as contribute to preventing the immune system from producing more new antibodies, minimizing the attack on cells. fetal red blood cells. From there, early screening and proactive preventive treatment will avoid giving birth to a child with severe jaundice leading to brain damage.Prevention is always the best. However, if it is too late and the infant has congenital hemolysis, the baby needs to be closely monitored for jaundice as well as a quantitative test of bilirubin in the blood, which helps to keep the baby within a safe range until the baby is born. when the liver can completely eliminate bilirubin out. If severe hemolysis leads to anemia, the neonate should be given an early blood transfusion with an appropriate volume. At the same time, children are also given light therapy to quickly eliminate bilirubin. In addition, the intensive care regimen such as increasing feeding time, increasing the amount of milk per feeding also helps to increase the amount of feces and urine, increasing the rate of bilirubin excretion.
To prevent complications caused by blood group incompatibility between mother and child, pregnant women should have pre-pregnancy examination and screening to help proactively and early detect risk factors affecting the health of mother and baby. In particular, in case the first birth has a phenomenon of ABO blood group incompatibility, women should give birth for the second time away from the first time to reduce the amount of antibodies in the body, which will be better for pregnancy and should be avoided. Consider choosing a package of prenatal care packages to closely monitor and minimize complications affecting mother and baby from the time of pregnancy to the time of labor.
At Vinmec International General Hospital, there is a package maternity service as a solution to help pregnant women feel secure because of the companionship of the medical team throughout the pregnancy. When choosing Maternity Package, pregnant women can:
The pregnancy process is monitored by a team of qualified doctors Regular check-up, early detection of abnormalities Maternity package helps to facilitate the process. birthing process Newborns get comprehensive care
MORE:
Blood group test during pregnancy: What to know Blood type disagreement during pregnancy: What to know What happens if there is rh blood group incompatibility between mother and baby? Recommended video:
Vinmec cord blood bank - solution for patients with serious diseases