This is an automatically translated article.
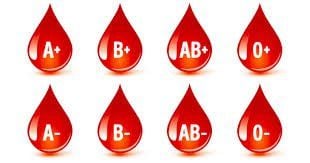
Most of us know the common blood types including A, B, AB, O. In each blood group, there is a plus and minus blood group system. Each person at birth has inherited genetics from their parents, so they have 1 of the 8 blood group systems mentioned above and do not change throughout life.
1. Mother has Rh- blood group, why is it dangerous for the fetus?
The plus and minus sign of each blood type indicates that the surface of the person's red blood cells has Rh antigen, written in full as Rh(D)+ in the first case or without Rh antigen, written in full as Rh( D)- in the second case.
In Vietnam, up to 99.96% of people are Rh+ (or O+ or B+ or A+ or AB+, in descending order) but only 0.04%- 0.07% of people are Rh- (or O- or B- or A- or AB-). Blood group with the ratio less than 0.1% is a rare blood group and less than 0.01% is a very rare blood group. People with rare blood type Rh- in our country belong to the community of people with rare blood type, statistics show that out of 10,000 people, only 4-7 people have Rh- blood type.
Being in a rare blood group puts this person at a much higher risk than others for a number of reasons:
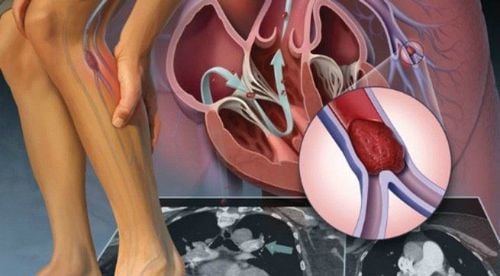
When a blood transfusion is urgently needed in cases of accidents, emergency surgery... This blood type is not always available for transfusion in hospitals and medical facilities. In case the mother has Rh- blood group, and the father has Rh+ blood group, according to the genetic rule, at least 50% of the children born will have the same Rh+ blood group as the father. In the first pregnancy, the child with the same Rh + blood type as the father develops normally until birth if the placental pregnancy process is not damaged. However, in the second pregnancy, if the child still has RH + blood group, there will often be a blood group incompatibility with the mother's blood type, which is Rh-. The mother's body produces antibodies that cross the placenta against the Rh+ antigen in the baby's blood group, causing red blood cell agglutination, also known as hemolysis. Consequences may cause miscarriage, stillbirth, premature birth, infants born with intellectual disabilities, hemolysis, frequent blood changes, etc. For women with Rh- blood group, there is a pregnancy group. Rh+ blood can have a blood transfusion accident right at the first Rh+ blood donation.

Không phải lúc nào nhóm máu Rh- này cũng có sẵn để truyền tại các bệnh viện và các cơ sở y tế
It is possible to talk more about the case of people with Rh blood group - that is, the body does not have the antigens of the Rh blood group, so it cannot fight against the antigens of the Rh group. The body may be sensitive to this blood group. The specific expression is obvious in pregnant women who receive blood transfusions that will produce antibodies against Rh +. From the second blood transfusion with Rh + group, in the body of people with Rh- blood group, there will be a reaction between antibodies and Rh antigens and cause immunity causing hemolysis.
In a simpler way, the mother with Rh- blood group has never received a blood transfusion, during pregnancy, often has the same blood group as the father, Rh+, the baby's red blood cells carrying the Rh+ blood type enter the mother's blood, stimulate induces the mother's body to produce anti-Rh+ antibodies. During the second pregnancy, this antibody can be transmitted to the fetus, against the baby's red blood cells, causing complications such as edema and hemolysis in the newborn.
2. How to prevent harm to the fetus due to RH- blood type?

Cần biết bản thân mình mang nhóm máu gì, nếu thuộc các nhóm máu hiếm cần có tâm lý sẵn sàng chuẩn bị trường trường hợp xấu nhất khi cần truyền máu
The seriousness of disagreement between Rh+ and Rh- groups requires us to understand and take measures to prevent and reduce the risk of harm to the fetus during pregnancy. You need to know what blood type you have, if you are of rare blood types, you need to be ready to prepare for the worst case scenario when you need a blood transfusion. Especially for women with Rh- blood group, it is necessary to manage and monitor pregnancy closely and properly. Pregnant women with Rh- blood group need anti-D prophylaxis if husband has RH+ blood group. Use of D-immune antibodies should be carried out under the advice of a doctor:
Monitor fetal anemia and the effectiveness of anti-D immune antibodies every 2 weeks for pregnant women; If anti-D immune antibody titers are negative, periodic prophylaxis with anti-D is recommended.
The use of anti-D is as follows: During pregnancy: there are 2 ways to use and the effect is similar;
Method 1: 2 doses of anti-D IgG 500 IU - 625 IU at week 28 and 34 of pregnancy (If anti-D is injected at week 28, week 34 can be injected with anti-D without having to do an effective test. price of immune antibodies). Method 2: inject a single dose of anti-D IgG 1500 IU at 28 weeks of pregnancy. Besides, it is also necessary to prevent postpartum, anti-D IgG 500IU - 1500 IU injection within 72 hours after birth (if the baby is born with Rh(D) positive blood group).
By having a pregnant mother with RH- blood group, the risk of danger to the fetus is minimized, ensuring the safety and development of the fetus.
At Vinmec International General Hospital, there is a package maternity service as a solution to help pregnant women feel secure because of the companionship of the medical team throughout the pregnancy. When choosing Maternity Package, pregnant women can:
The pregnancy process is monitored by a team of qualified doctors Regular check-up, early detection of abnormalities Maternity package helps to facilitate the process. birthing process Newborns receive comprehensive care.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.