This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
In patients with chronic atrophic gastritis, in addition to vitamin B12 deficiency, iron deficiency anemia (IDA) may precede or overlap with age being an important factor that manifests first.
1. What is atrophic gastritis?
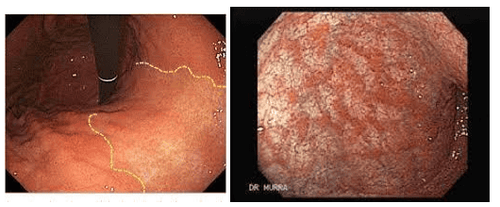
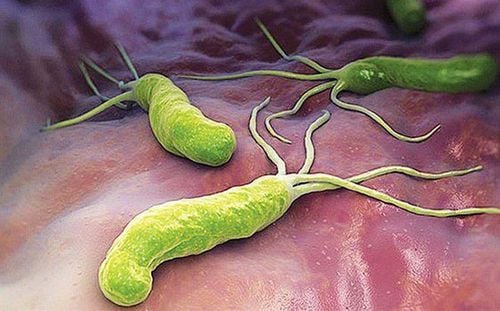
Atrophic gastritis is a disease caused by H. pylori bacteria that destroy the mucosa after a long time. Gastric mucosal atrophy is a condition characterized by chronic inflammation in which gastric glandular cells are lost and replaced by intestinal mucosal epithelium, pyloric and fibrous stroma.
Patients with end-stage chronic gastritis will become atrophic gastritis. But there are also some cases of autoimmune atrophic gastritis, when the immune system attacks healthy mucosal cells due to an error in the body. That's called autoimmune atrophic gastritis.
2. Consequences of atrophic gastritis
Atrophic gastritis is a disease caused by H. pylori bacteria that destroy the mucosa after a long time. Gastric mucosal atrophy is a condition characterized by chronic inflammation in which gastric glandular cells are lost and replaced by intestinal mucosal epithelium, pyloric and fibrous stroma.
Patients with end-stage chronic gastritis will become atrophic gastritis. But there are also some cases of autoimmune atrophic gastritis, when the immune system attacks healthy mucosal cells due to an error in the body. That's called autoimmune atrophic gastritis.
Chronic atrophic gastritis (atrophic gastritis) leads to destruction of gastric mucosal parietal cells leading to decreased gastric acid secretion and decreased intrinsic factor (IF) production. The consequences of this are increased stomach pH (decreased acidity), hyperglycemia, and intrinsic factor deficiency.
As a result, chronic atrophic gastritis can lead to malabsorption (albeit by different mechanisms) of vitamin B12 and iron, causing megaloblastic or iron deficiency anemia. . Vitamin B12 deficiency, due to decreased intrinsic factor production, can lead to giant cell anemia and various neurological dysfunctions. The mechanism of iron deficiency in chronic atrophic gastritis is less clear, but may be due to decreased acid secretion or co-infection with Helicobacter pylori. In addition, deficiencies of other vitamins and micronutrients (such as vitamin D, calcium, and vitamin C) have been known to occur in patients with chronic atrophic gastritis, although the mechanisms for these This has been studied less.
3. Why is there atrophic gastritis?
Chronic atrophic gastritis leads to atrophy of the gastric body mucosa and chronic loss of gastric parietal cells. These parietal cells, under the influence of gastrin (from G cells) and histamine (from ECL cells), stimulate acid production and lead to a decrease in pH in the gastric lumen. Parietal cells also control intrinsic factor (intrinsic factor) production by a different mechanism. This loss of parietal cells results in decreased gastric acid secretion and decreased intrinsic factor production.
The cause of atrophic gastritis (AG) is (i) immune-mediated destruction by antibodies (intrinsic factor and/or parietal cells) against the gastric mucosa (known as inflammation of the stomach lining). Chronic autoimmune gastric atrophy or (ii) Helicobacter pylori (H. pylori infection) Regardless of the cause, the net effect of parietal cell loss and gastric atrophy is decreased acid secretion. In populations at low risk of gastric cancer (as in the US), endoscopic surveillance every 3 years is recommended for patients with extensive atrophic gastritis or intestinal metaplasia.
4. Iron deficiency in patients with chronic atrophic gastritis
In patients with chronic atrophic gastritis, in addition to vitamin B12 deficiency, iron deficiency anemia (IDA) may precede or overlap with age being an important factor that manifests first. Younger patients are more likely to develop features of iron deficiency anemia while those over 60 years of age tend to have massive vitamin B12 deficiency.
Age-dependent anemia presentation in patients with chronic atrophic gastritis reflects a higher prevalence of active H. pylori infection in younger patients. As a result, red blood cell indices such as mean cell volume (MCV) may not be reliable in patients with chronic atrophic gastritis, as there may be two distinct or overlapping pathologies (may be present). mean cell volume increased and mean cell volume decreased), so it appeared within the normal range. A possible role of decreased acid secretion in the development of iron malabsorption has been suggested in different models of acid reduction/reduction. Low gastric acid secretion is the result of parietal cell loss. This low production of stomach acid leads to a decrease in the solubility of iron in food and a decrease in iron absorption. Thus, iron deficiency anemia is a common manifestation of chronic atrophic gastritis, but is often overlooked.
>> See also: Vitamin D, C and calcium deficiency in patients with chronic atrophic gastritis – Posted by Master, Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec International General Hospital Central Park
5. Must find and treat H. pylori in patients with iron deficiency anemia due to chronic atrophic gastritis
In a study of 160 patients diagnosed with autoimmune gastritis due to the combined presence of hyperglycemia and strong antimalarial cell antibodies, 83 (52%) had anemia due to Iron deficiency manifested by low serum ferritin levels, low transferrin saturation and microcytic anemia of iron deficiency anemia due to H. pylori infection in patients with more complicated chronic atrophic gastritis. It has been shown that up to two-thirds of patients with atrophic gastritis have evidence of H. pylori infection. This high prevalence suggests that infection may have a specific role in the disease rather than a mere association. Therefore, it is essential that H. pylori be actively excluded in all patients with chronic atrophic gastritis (or pernicious anemia), so as not to miss concomitant iron deficiency anemia .
It was also observed that the non-response to oral iron therapy was more than twice as high in H. pylori-positive patients as in H. pylori-negative patients, suggesting that H. pylori infection alters response to oral iron therapy in iron-deficiency anemia.
Healing of H. pylori infection is associated with reversal of iron dependence and recovery from iron deficiency anemia. Therefore, eradication of H. pylori, together with iron replacement, is essential in the management of patients with chronic atrophic gastritis and iron deficiency anemia. H.pylori is treated with active eradication in all patients with chronic atrophic gastritis (or pernicious anemia), so as not to miss iron-deficiency anemia.
In summary, atrophic gastritis, regardless of its cause, leads to nutritional deficiencies through parietal cell atrophy and, as a result, decreased acid secretion. Vitamin B12 deficiency is well described, but is often diagnosed late. A patient with unexplained iron deficiency anemia should be excluded from atrophic gastritis (and concurrent H. pylori). The importance of vitamin D, calcium and vitamin C malabsorption in chronic atrophic gastritis remains to be seen.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease, inflammatory bowel disease.. Along with that, at Vinmec Hospital, screening for stomach cancer and gastric polyps is done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging) function. narrow light frequency) results in clearer mucosal pathological analysis results than conventional endoscopy, detection of ulcerative colitis lesions, early gastrointestinal cancer lesions... Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can be assured of gastroscopy and esophagogastroduodenoscopy services here. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Gluckman CR, Metz DC. Gastric neuroendocrine tumors (Carcinoids). Current Gastroenterology Reports (2019) 21:13. 2.Sato Y. Clinical features and management of gastric carcinoid type 1. Clin J Gastroenterol (2014) 7: 381386.
Lahner E, Carabotti M, Annibale B. Atrophic gastritis: Manifestations, diagnosis and clinical outcomes. EMJ Gastroenterol. 2017; 6 [1]: 75-82. Bank M, Graham D, Jansen M, et al British Gastroenterology Society guidelines for the diagnosis and management of patients at risk for gastric adenocarcinoma. Intestine. September 2019; 68 (9): 1545-1575.